Discharge Summary Template
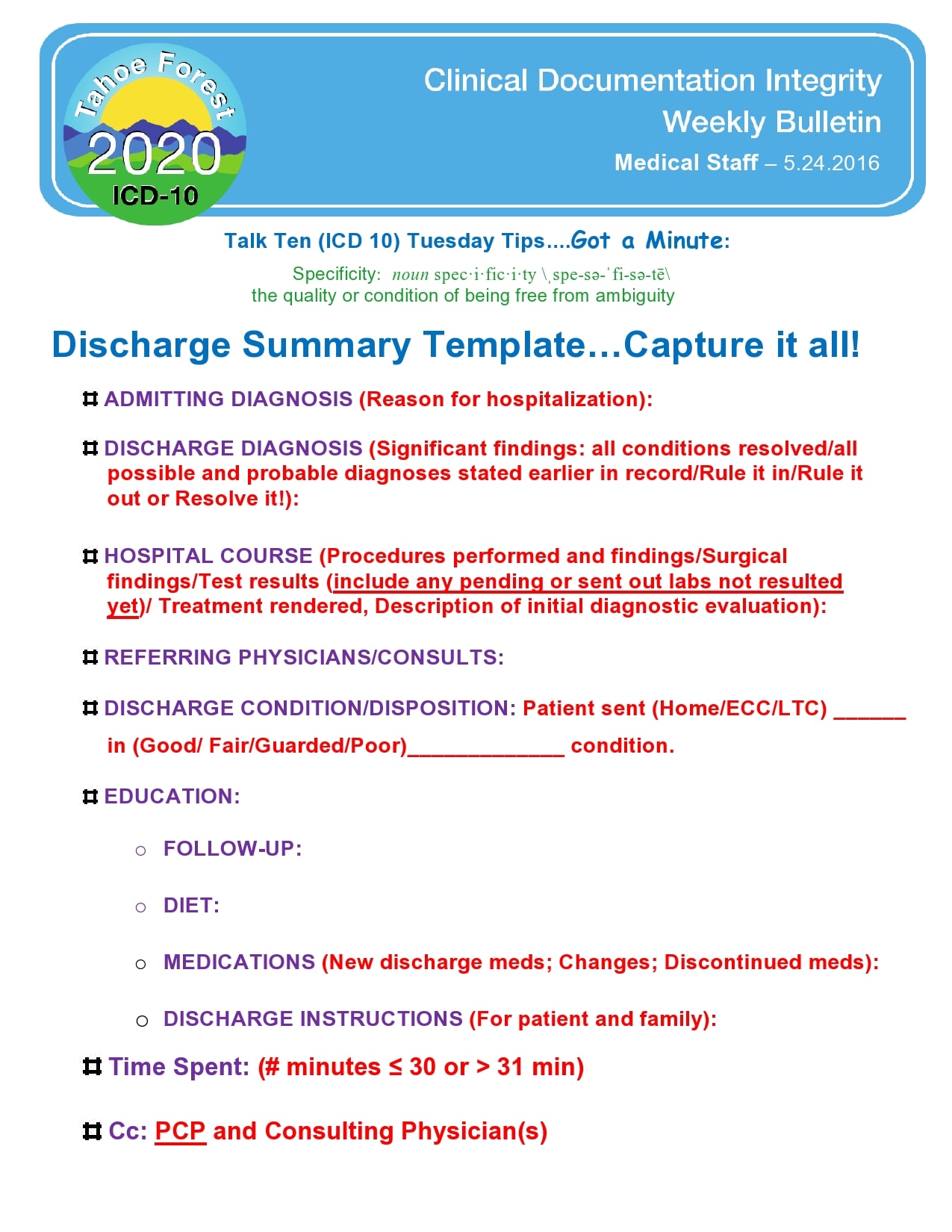
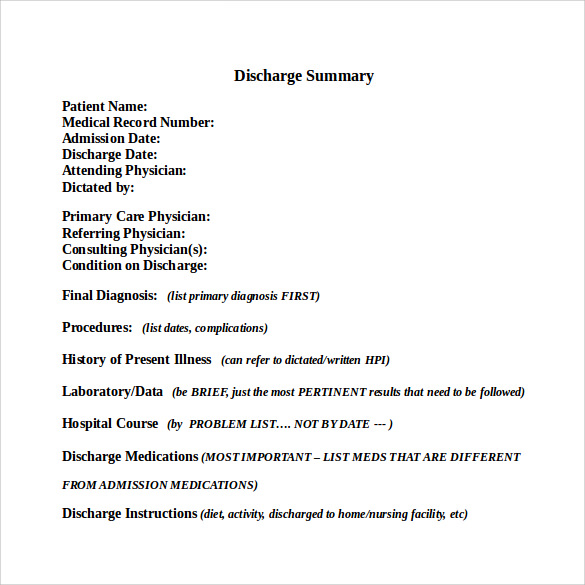
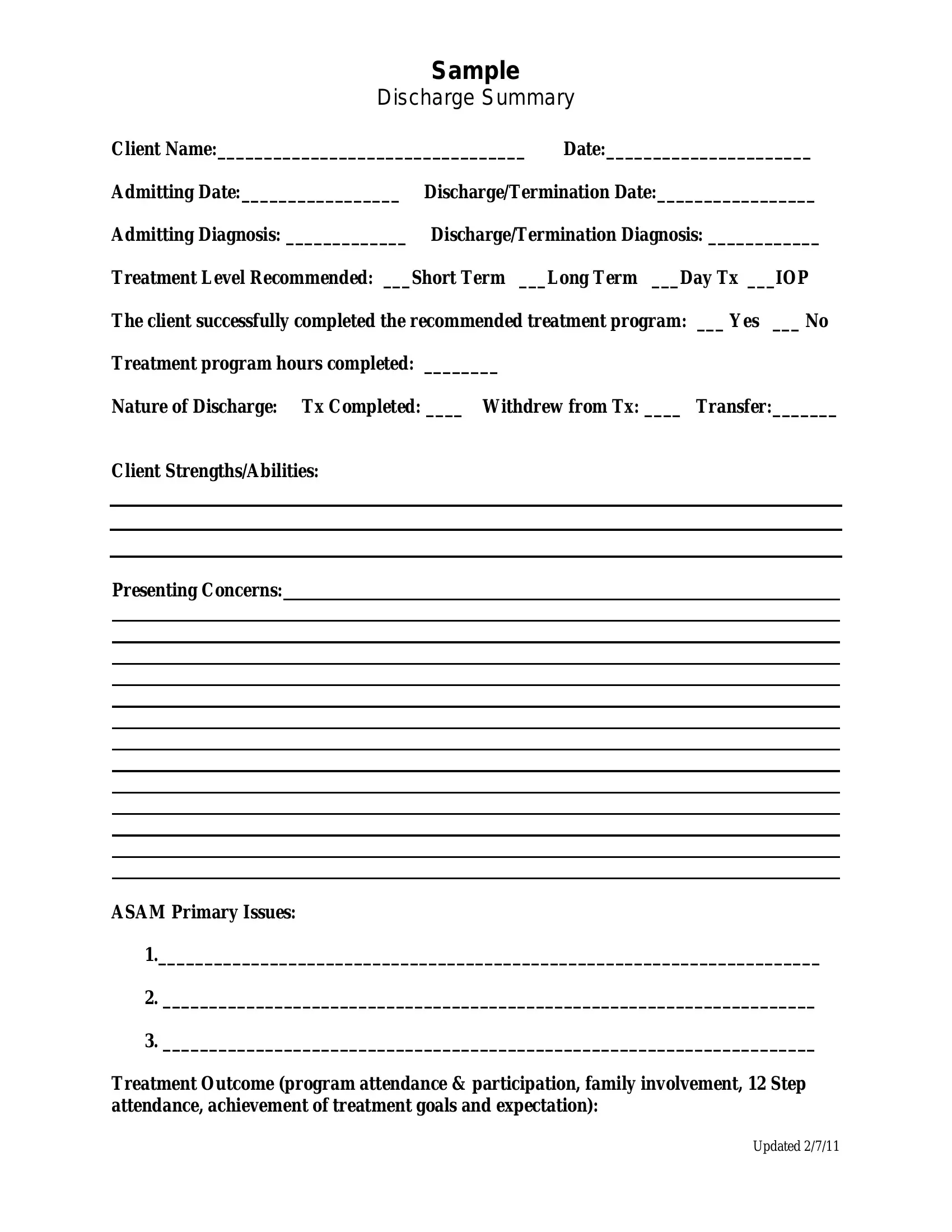
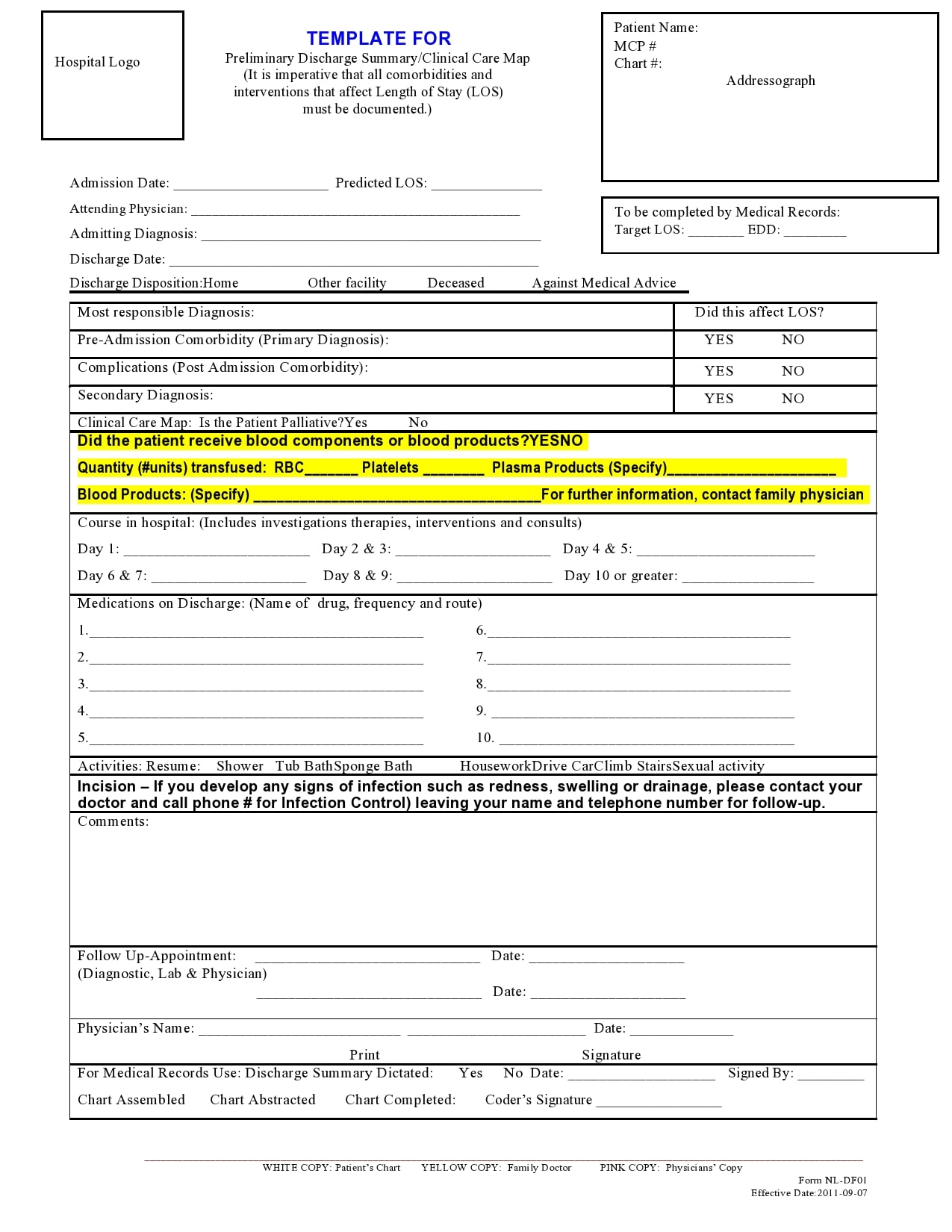
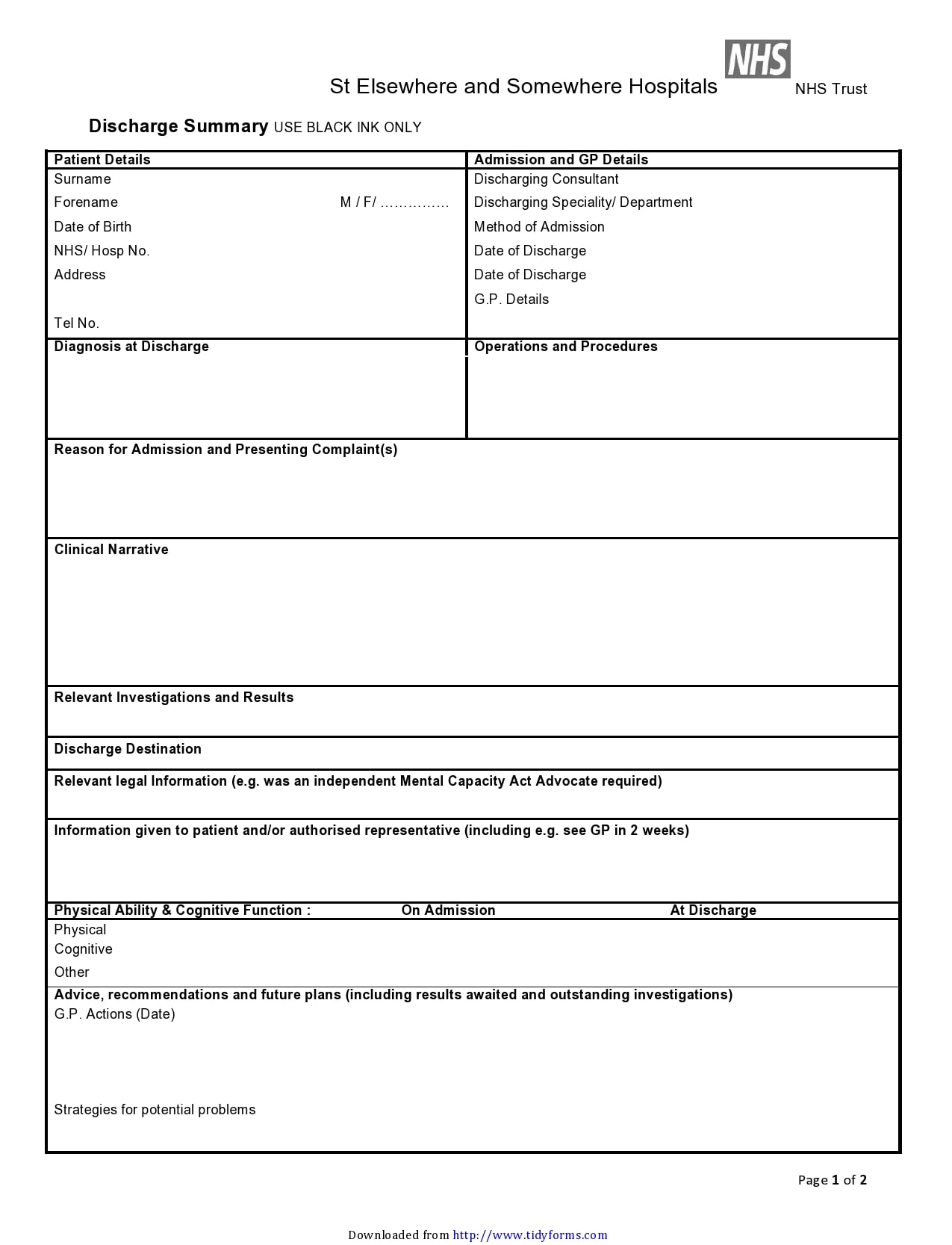
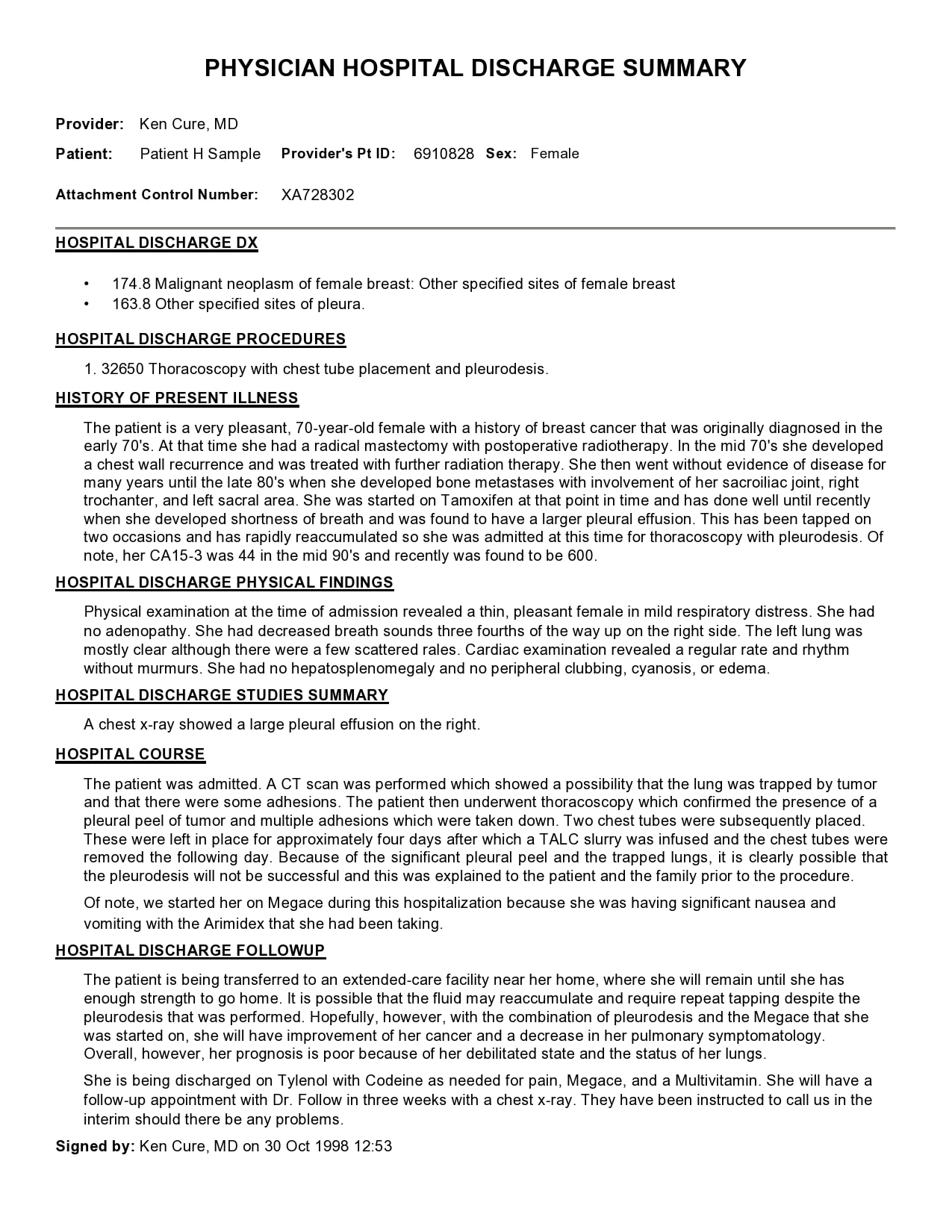
Discharge Summary Template - Web in 2014, the british society of gastroenterology (bsg) published a standards framework outlining key performance indicators for ercp practitioners and services. In the last 10 years there have been numerous changes to clinical practice yet there remains considerable variation in service delivery in the uk. Let’s review how to create effective discharge summaries and create a standardized template to enhance documentation practices among healthcare professionals. Web a total of 20 physicians who practice outpatient general internal or family medicine in california participated in a recent study. Web a discharge summary template is a medical report written by a health professional after treatment or at the end of the patient’s stay in the hospital. Web discharge summary forms are usually completed during a patient’s hospital stay and contain essential medical information about the care they received, including details about allergies, medications, and clinical findings. The document is essential for: Compile patient medical records and treatment details. Once all information is reviewed and deemed accurate, finalize the discharge summary. Obtain preliminary report from the attending physician. Web a discharge summary template is a document that summarizes the hospital encounter of a patient and identifies encounters, care processes provided, and progress and discharge instructions. Physician's review of preliminary discharge summary. Incorporate review feedback into the discharge summary. Web a discharge summary is a handover document that explains to any other healthcare professional why the patient was admitted, what has happened to them in hospital, and all the information that they need to pick. Compile patient medical records and treatment details. It may contain crucial data like the patient’s identity, admission and discharge dates, diagnosis and prognosis, medication records, treatment regimen. Web discharge summaries are essential documents that ensure continuity of care from hospital to outpatient settings. This document facilitates continuity of. Consultation submission has now closed and the review is underway. This template will assist healthcare and medical professionals working in primary care or hospitals complete the online consultation. In the last 10 years there have been numerous changes to clinical practice yet there remains considerable variation in service delivery in the uk. University health network discharge summary template for dictation. Avoid allegations of abandonment with our expert guidance. Web if a client needs to be referred to a new level of care (e.g., from outpatient to inpatient, or to a specialized facility), the discharge summary helps to communicate the treatment history, reason for referral, and any relevant information for the new care team. Discharge summary) in an osce setting. Include feeding regimen if child is on tube feeds, or include if there has been a formula change. Web a discharge summary template is a medical report written by a health professional after treatment or at the end of the patient’s stay in the hospital. Web a discharge summary is a comprehensive clinical report prepared by healthcare professionals when a patient is discharged from a hospital or other health care settings. In 2021 the bsg commissioned an. Assisting in clinical decision making. Otherwise, you can skip this. Avoid allegations of abandonment with our expert guidance. Web our free summary discharge template is easy to use and highly customizable to suit the specific needs of various healthcare scenarios, offering flexibility and adaptability. The study’s findings have implications for improving the continuity of care and enhancing communication between hospitalists and primary care physicians. The. Web explore a detailed guide on a discharge summary, its requirements, examples, and a free downloadable template to streamline patient care transitions. Include medication name, dose, route, frequency, duration of therapy if acute. Web if a client needs to be referred to a new level of care (e.g., from outpatient to inpatient, or to a specialized facility), the discharge summary. Assisting in clinical decision making. Web if a client needs to be referred to a new level of care (e.g., from outpatient to inpatient, or to a specialized facility), the discharge summary helps to communicate the treatment history, reason for referral, and any relevant information for the new care team. Otherwise, you can skip this. In 2021 the bsg commissioned. In general, this document is the main mode of communication between the healthcare team of the hospital and the providers of aftercare. It may contain crucial data like the patient’s identity, admission and discharge dates, diagnosis and prognosis, medication records, treatment regimen. The study’s findings have implications for improving the continuity of care and enhancing communication between hospitalists and primary. Web learn what a discharge note or discharge summary is for terminating therapy with your client. Include medication name, dose, route, frequency, duration of therapy if acute. University health network discharge summary template for dictation. This document facilitates continuity of. Web in 2014, the british society of gastroenterology (bsg) published a standards framework outlining key performance indicators for ercp practitioners. Once all information is reviewed and deemed accurate, finalize the discharge summary. Use our template to ensure a smooth termination process and maintain a positive therapeutic relationship. Web discharge summary forms are usually completed during a patient’s hospital stay and contain essential medical information about the care they received, including details about allergies, medications, and clinical findings. Web if a. Avoid allegations of abandonment with our expert guidance. Web a discharge summary template that allows users to fill and download the document in pdf or word format. Web the discharge summary template approved by the health authority medical advisory committee (hamac) provides a standard framework for physicians to consistently and effectively complete and communicate critical patient care information. As a. Let’s review how to create effective discharge summaries and create a standardized template to enhance documentation practices among healthcare professionals. Web a discharge summary is a handover document that explains to any other healthcare professional why the patient was admitted, what has happened to them in hospital, and all the information that they need to pick. Physician's review of preliminary. This document facilitates continuity of. Web learn what a discharge note or discharge summary is for terminating therapy with your client. They were interviewed about their experiences with discharge summaries and their perspectives on some commonly used summary templates. Web in essence, discharge summary templates are documents (usually printed) that contain all the health information pertaining to the patient’s stay. This document facilitates continuity of. Web a discharge summary template is a medical report written by a health professional after treatment or at the end of the patient’s stay in the hospital. Autonotes facilitates easy editing and formatting to ensure the document is professional and comprehensive. Web discharge summaries are essential documents that ensure continuity of care from hospital to. Draft a preliminary discharge summary. Include feeding regimen if child is on tube feeds, or include if there has been a formula change. They were interviewed about their experiences with discharge summaries and their perspectives on some commonly used summary templates. Web our free summary discharge template is easy to use and highly customizable to suit the specific needs of various healthcare scenarios, offering flexibility and adaptability. Web a discharge summary template is a medical report written by a health professional after treatment or at the end of the patient’s stay in the hospital. It may contain crucial data like the patient’s identity, admission and discharge dates, diagnosis and prognosis, medication records, treatment regimen. The document is essential for: University health network discharge summary template for dictation. The study’s findings have implications for improving the continuity of care and enhancing communication between hospitalists and primary care physicians. Once all information is reviewed and deemed accurate, finalize the discharge summary. Web discharge summary forms are usually completed during a patient’s hospital stay and contain essential medical information about the care they received, including details about allergies, medications, and clinical findings. Web if a client needs to be referred to a new level of care (e.g., from outpatient to inpatient, or to a specialized facility), the discharge summary helps to communicate the treatment history, reason for referral, and any relevant information for the new care team. In the last 10 years there have been numerous changes to clinical practice yet there remains considerable variation in service delivery in the uk. Create a detailed and professional discharge summary easily using this free template. Web a discharge summary is a comprehensive clinical report prepared by healthcare professionals when a patient is discharged from a hospital or other health care settings. Web discharge summaries are essential documents that ensure continuity of care from hospital to outpatient settings.30 Hospital Discharge Summary Templates (& Examples)
Discharge Summary Template Occupational Therapy Excel vrogue.co
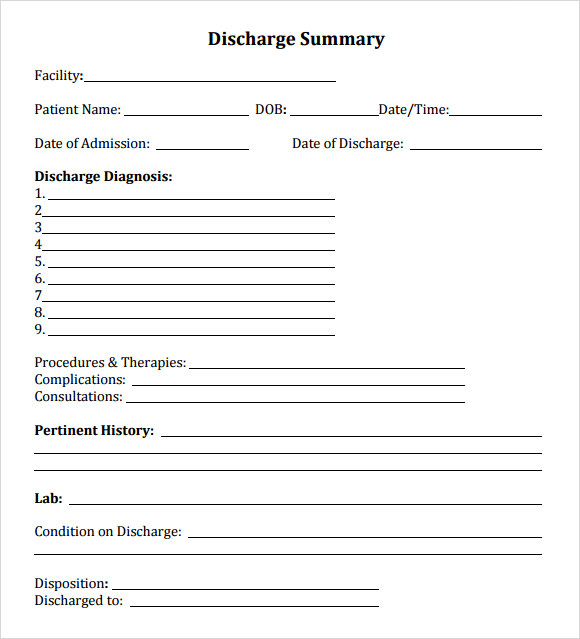
FREE 7+ Sample Discharge Summary Templates in PDF MS Word
30 Hospital Discharge Summary Templates (& Examples)
FREE 11+ Sample Discharge Summary Templates in PDF MS Word
FREE 11+ Sample Discharge Summary Templates in PDF MS Word
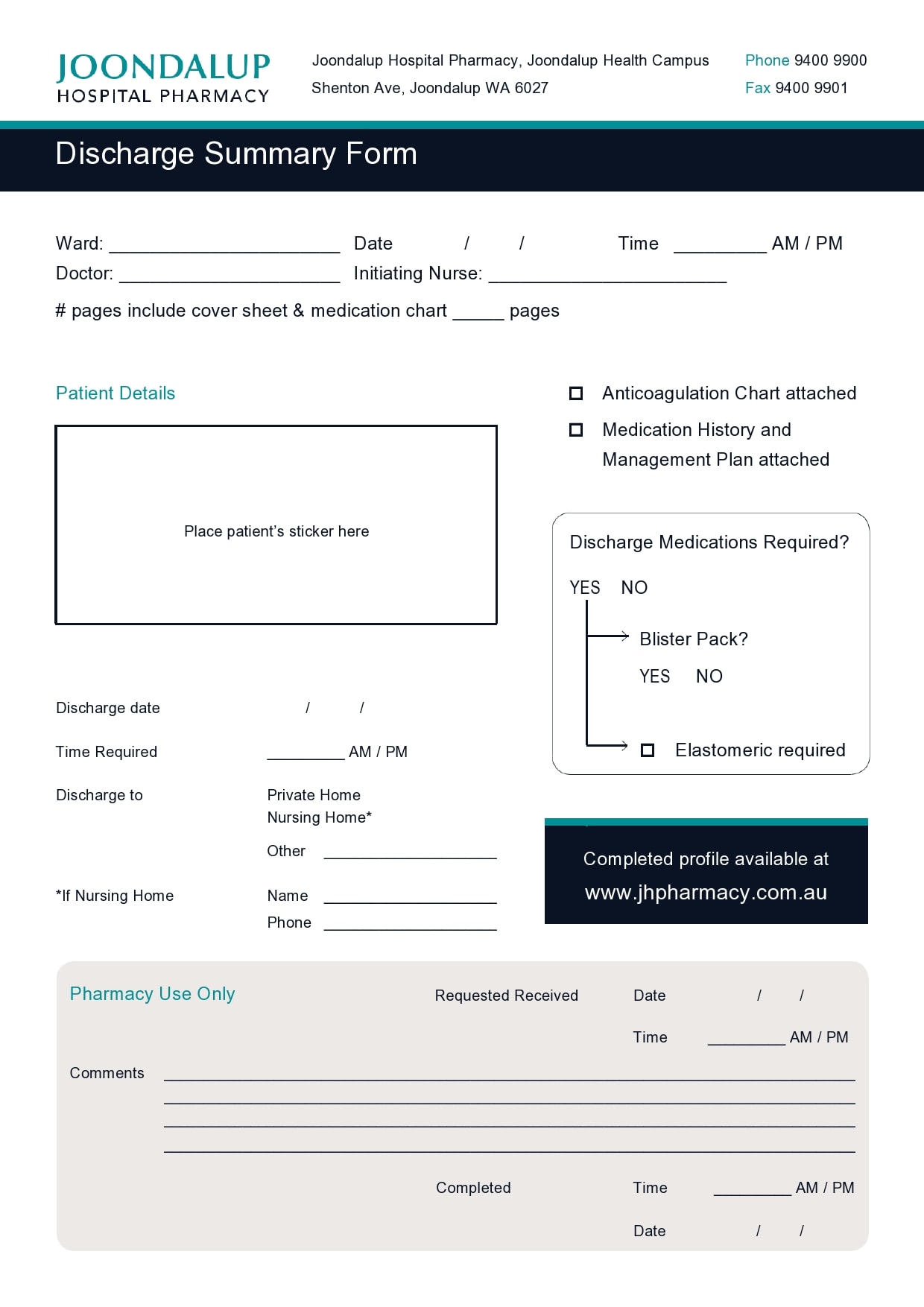
Discharge Summary Form ≡ Fill Out Printable PDF Forms Online
30 Hospital Discharge Summary Templates (& Examples)
30 Hospital Discharge Summary Templates (& Examples)
30 Hospital Discharge Summary Templates (& Examples)
Consultation Submission Has Now Closed And The Review Is Underway.
This Document Facilitates Continuity Of.
Incorporate Review Feedback Into The Discharge Summary.
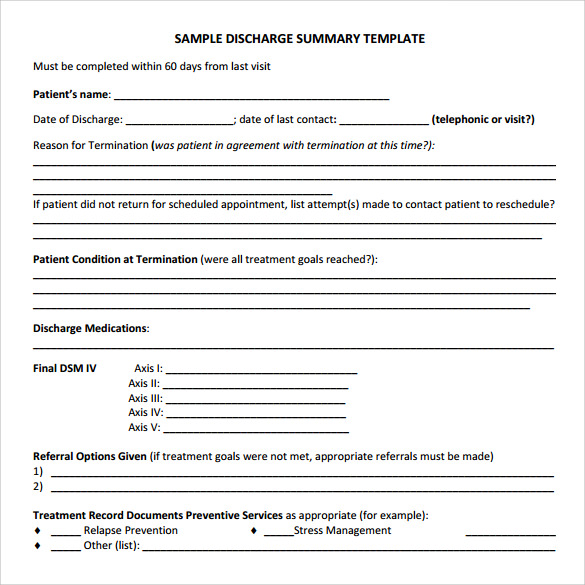
Web Learn What A Discharge Note Or Discharge Summary Is For Terminating Therapy With Your Client.
Related Post: