H And P Template
H And P Template - Emergency medicine • h&p template name: The rash in his diaper area is getting worse. history of present illness: It outlines the key sections to include such as the chief complaint, history of present illness, past medical history, review of systems, physical examination, assessment and plan. Adult h & p form. The following outline for the pediatric history and physical examination is comprehensive and detailed. I'll talk about why we created this notebook and compare it to the origi. U or iu, trailing zeros (1.0) or leading zeros (.1), ms or mso4, mgso4, da or dop, db, or dob, qd or qod, snp. She has never experienced this before. Web the written history and physical (h&p) serves several purposes: The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. It outlines a plan for addressing the issues which prompted the hospitalization. Adult h & p form. Can be pdf or notion or any other format! I'll talk about why we created this notebook and compare it to the origi. History & physical short form / procedure. The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Kenneth acha, md, ucr fm pgy2. Web this sample summative h&p was written by a second‐year medical student from ucf com class of 2020 at the end of cop‐2. Ucla form #201539 rev (10/14) page 1 of 1. Emergency medicine • h&p template name: Emergency medicine • h&p template name: She was first admitted to cpmc in 1995 when she presented with a complaint of intermittent midsternal chest pain. History & physical short form / procedure. Web the history and physical (h&p) form serves as a critical document in the medical field, intended to provide a comprehensive overview of an inpatient's medical history and current physical condition in settings like greenville hospital system. U or iu, trailing zeros (1.0) or leading zeros (.1), ms or mso4, mgso4, da or dop, db, or dob, qd or qod, snp. Ucla form #201539 rev (10/14) page 1 of 1. Include the dimensions of the chief complaint, including location, quality or character, quantity or severity, timing (onset, duration and frequency), setting in which symptoms occur, aggravating and alleviating factors and associated symptoms. Web this sample summative h&p was written by a second‐year medical student from ucf com class of 2020 at the end of cop‐2. History of tah/bso to keep track of all problems uncovered in the interview 5. Web this document provides a template for writing a history and physical examination report. I'll talk about why we created this notebook and compare it to the origi. “my mouth is numb.” hpi: Dyspnea final written h&p, (and just list a final problem list 3. History of tah/bso to keep track of all problems uncovered in the interview 5. Web history & physical (short form) date: The following outline for the pediatric history and physical examination is comprehensive and detailed. History of tah/bso to keep track of all problems uncovered in the interview 5. I'll talk about why we created this notebook and compare it to the origi. History & physical short form / procedure. Kenneth acha, md, ucr fm pgy2. I highly recommend you use them to notate your h&p and anesthetic plan for your cases. The history was obtained from both the patient’s mother and grandmother, who are both considered to be reliable historians. She was first admitted to cpmc in 1995 when she presented with a complaint of intermittent midsternal chest pain. Web websites with helpful h&p information.. The following outline for the pediatric history and physical examination is comprehensive and detailed. It outlines the key sections to include such as the chief complaint, history of present illness, past medical history, review of systems, physical examination, assessment and plan. Dyspnea final written h&p, (and just list a final problem list 3. Is an 83 year old retired nurse. I highly recommend you use them to notate your h&p and anesthetic plan for your cases. History & physical short form / procedure. Ja is a 79 year old white female who came in today due to numbness of the lip and mouth. Can be pdf or notion or any other format! Web h & p example. Web history and physical examination (h&p) examples. History of htn (4 years) shown below), it is useful to make an initial list simply 4. Web h & p example. The students have granted permission to have these h&ps posted on the website as examples. Kenneth acha, md, ucr fm pgy2. Web history & physical short form / procedure. H&p is shorthand for the formal document that physicians produce through the interview with the patient, the physical exam, and the summary of the testing either obtained or pending. History of htn (4 years) shown below), it is useful to make an initial list simply 4. The students have granted permission to. Date and time of h&p: The history was obtained from both the patient’s mother and grandmother, who are both considered to be reliable historians. Kenneth acha, md, ucr fm pgy2. Can be pdf or notion or any other format! It outlines the key sections to include such as the chief complaint, history of present illness, past medical history, review of. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Adult h & p form. Ja is a 79 year old white female who came in today due to numbness of the lip and mouth. Web the process of taking a history and performing a physical examination (h&p) in. ① always start with the patient’s age, chief complaint and vital signs cc: Adult h & p form. Web history of present illness: Web history and physical examination (h&p) examples. The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Include the dimensions of the chief complaint, including location, quality or character, quantity or severity, timing (onset, duration and frequency), setting in which symptoms occur, aggravating and alleviating factors and associated symptoms. Web the process of taking a history and performing a physical examination (h&p) in ob/gyn patients presents unique challenges. Web adult history & physical note. Can be pdf or notion or any other format! I highly recommend you use them to notate your h&p and anesthetic plan for your cases. Web websites with helpful h&p information. It outlines the key sections to include such as the chief complaint, history of present illness, past medical history, review of systems, physical examination, assessment and plan. She first experienced this today after her morning cup of coffee when she felt the left side of her mouth and lip go to sleep. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Ja is a 79 year old white female who came in today due to numbness of the lip and mouth. While not perfect, it best exemplifies the documentation skills students are expected and able to acquire by the end of p‐2: The students have granted permission to have these h&ps posted on the website as examples. The rash in his diaper area is getting worse. history of present illness: Adult h & p form. Date and time of h&p:DIGITAL Download, Printable Essential H&P Clinical Template for Medical
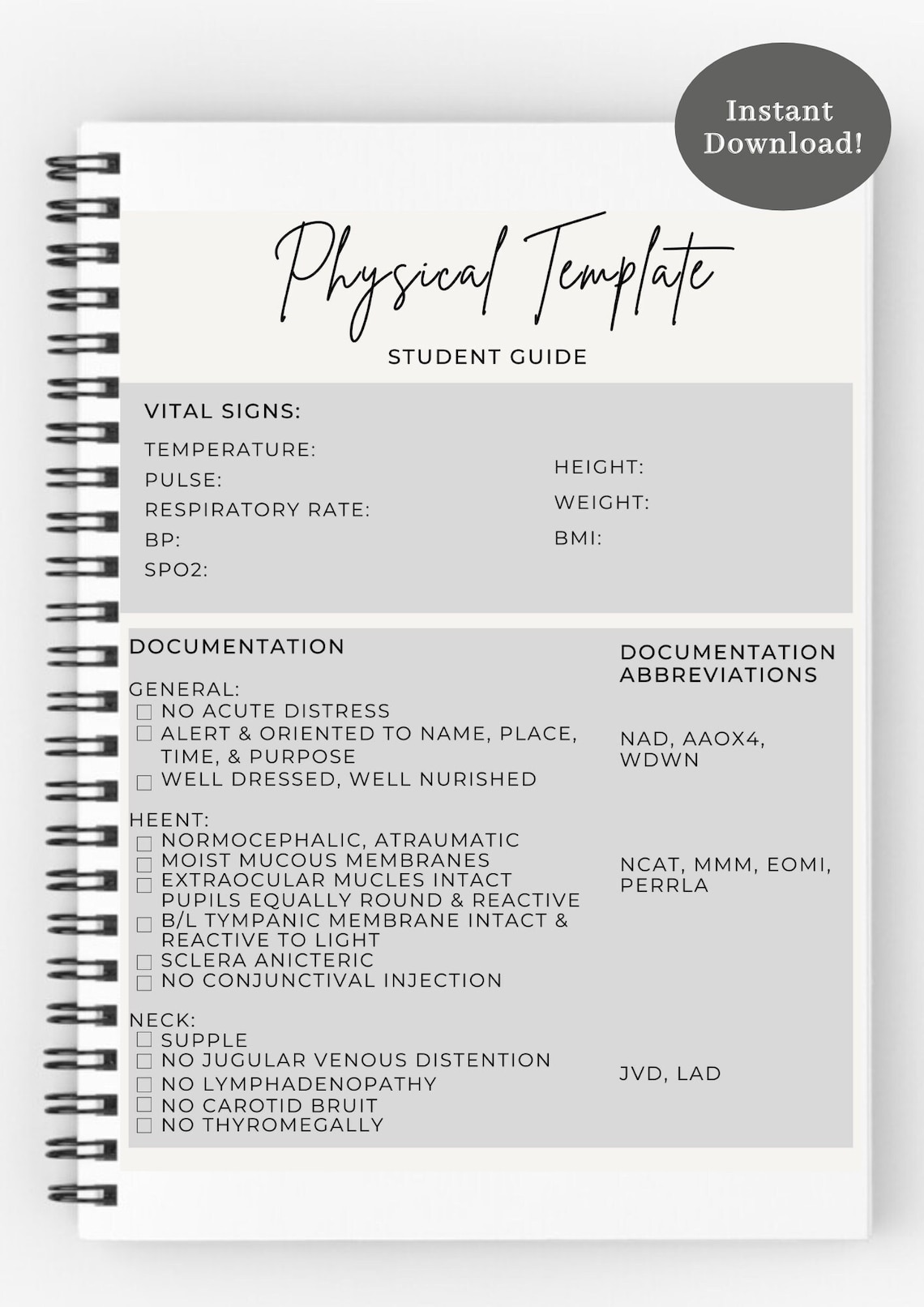
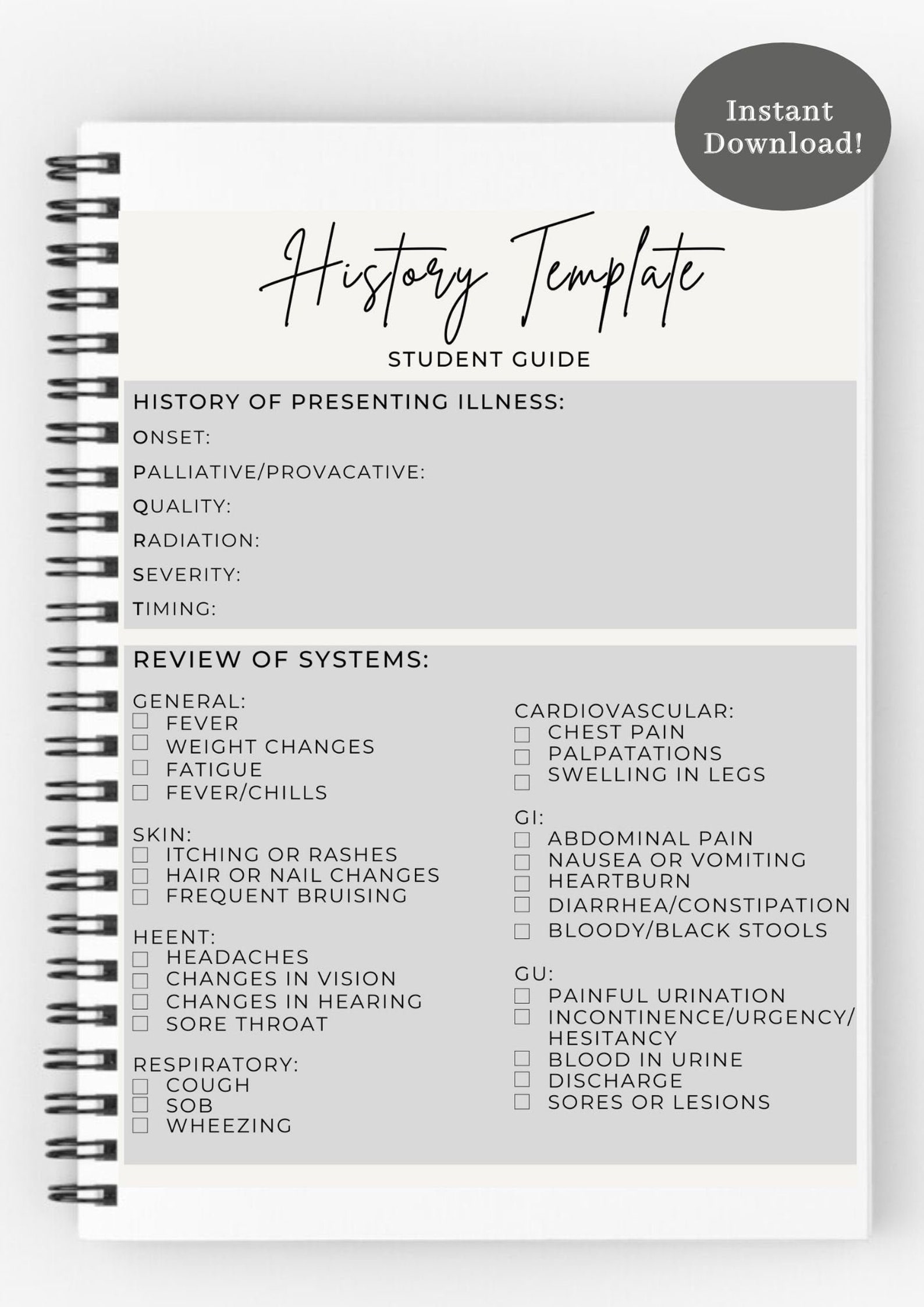
Printable Blank H&P Template
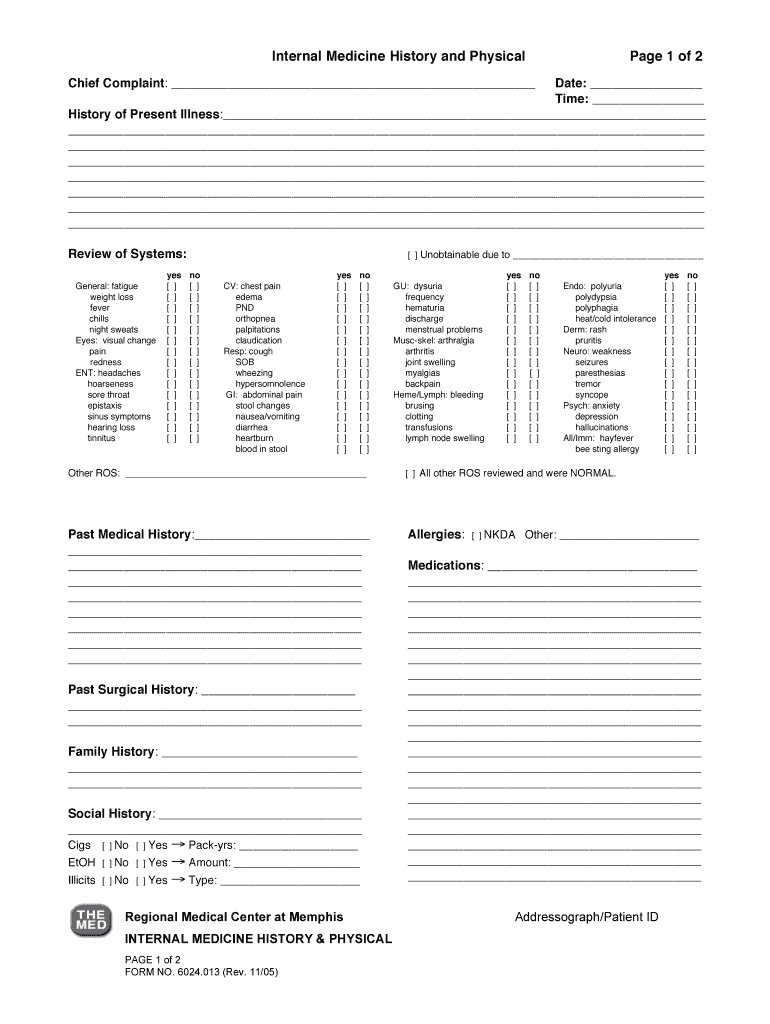
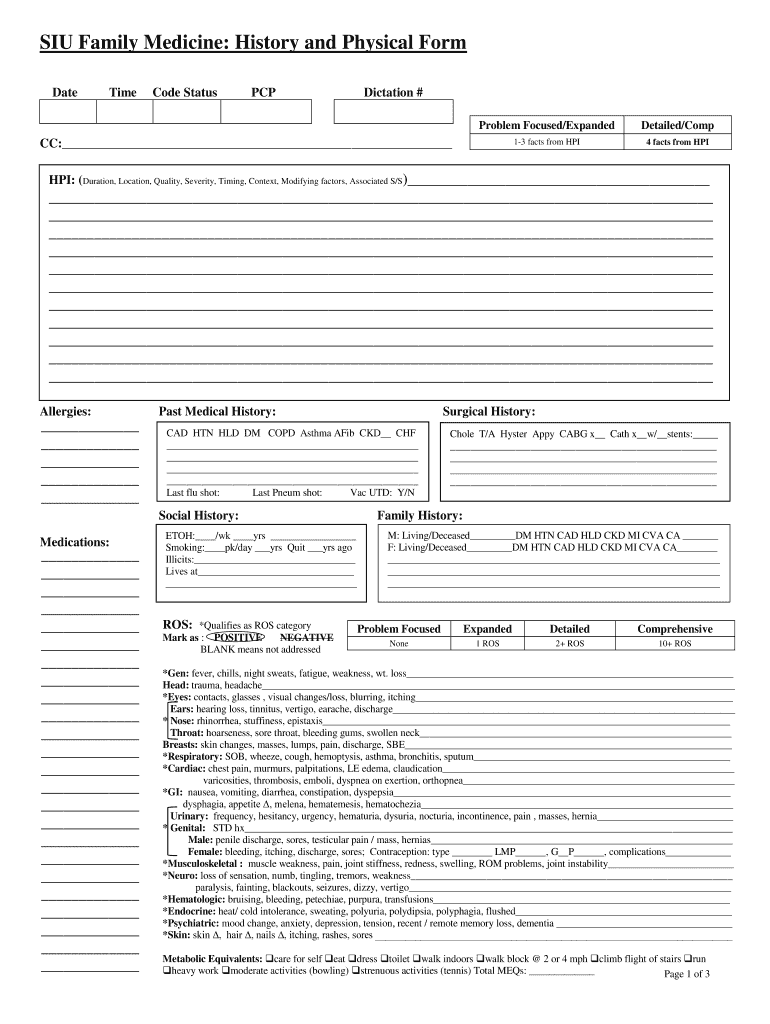
H P Template Fill Online, Printable, Fillable, Blank pdfFiller
H P Template Fill Online, Printable, Fillable, Blank throughout
DIGITAL Download, Printable Essential H&P Clinical Template for Medical
History and physical template Fill out & sign online DocHub
Printable H&P Template
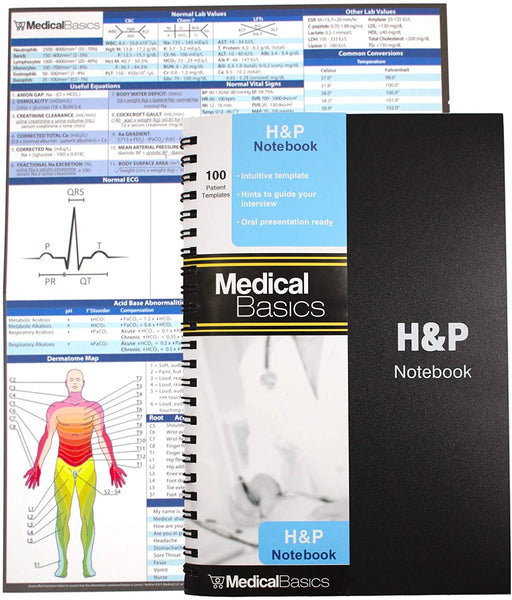
H&P Template Notebook Medical History and Physical 100 Templates with
History and physical template Fill out & sign online DocHub
[Clinical] H&P Template for Pocket Medicine r/medicalschool
Web Sample Pediatric History And Physical Exam.
History & Physical Short Form / Procedure.
“My Mouth Is Numb.” Hpi:
Web This Document Provides A Template For Writing A History And Physical Examination Report.
Related Post:




![[Clinical] H&P Template for Pocket Medicine r/medicalschool](https://external-preview.redd.it/8bi15gs5EgSlBZLSb8o1wNfO-2Ux1e9xXZzIu5Ha7ss.jpg?auto=webp&s=c391dd104fadbebca56c1003a71f41960ee9d00e)