History And Physical Template
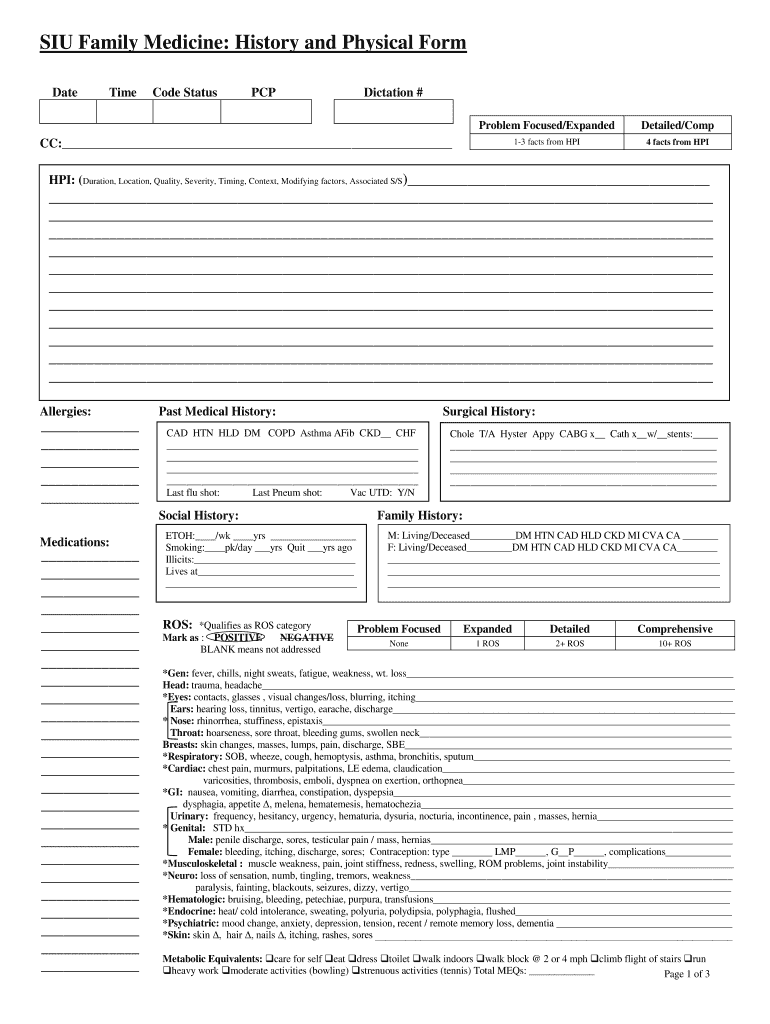
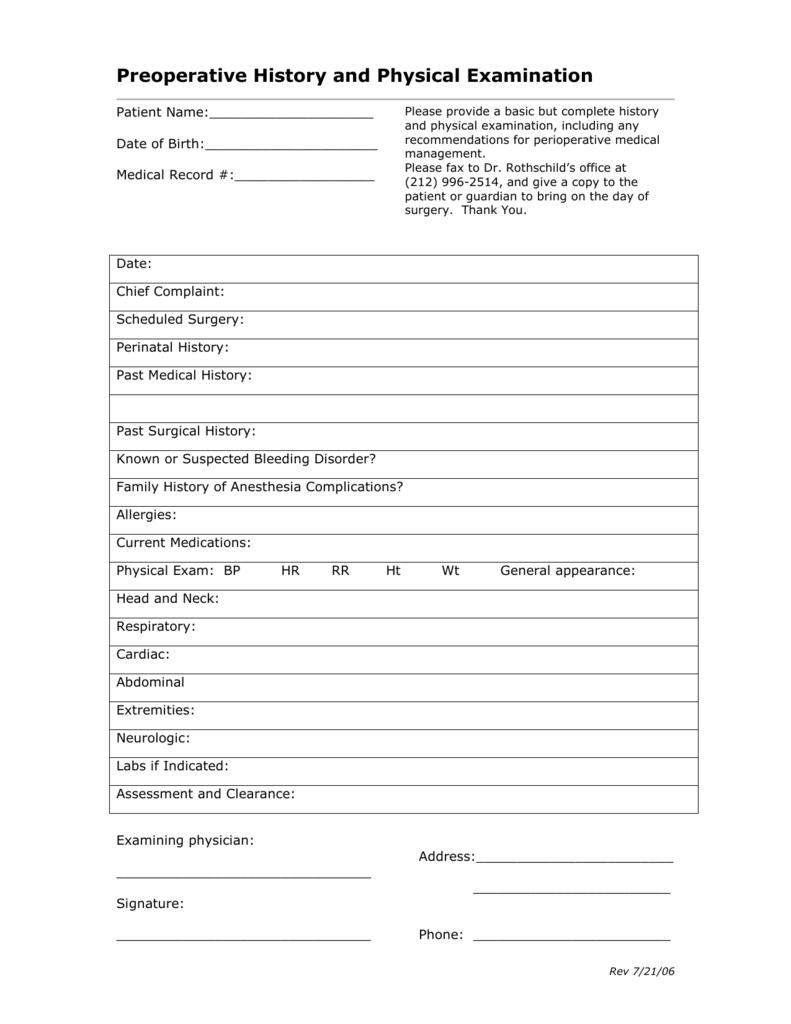
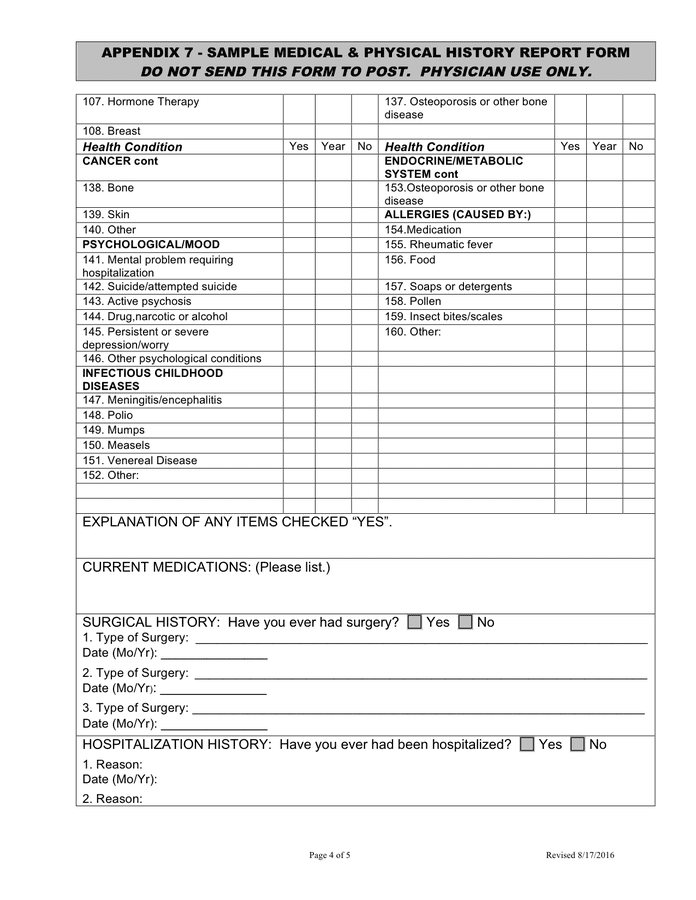
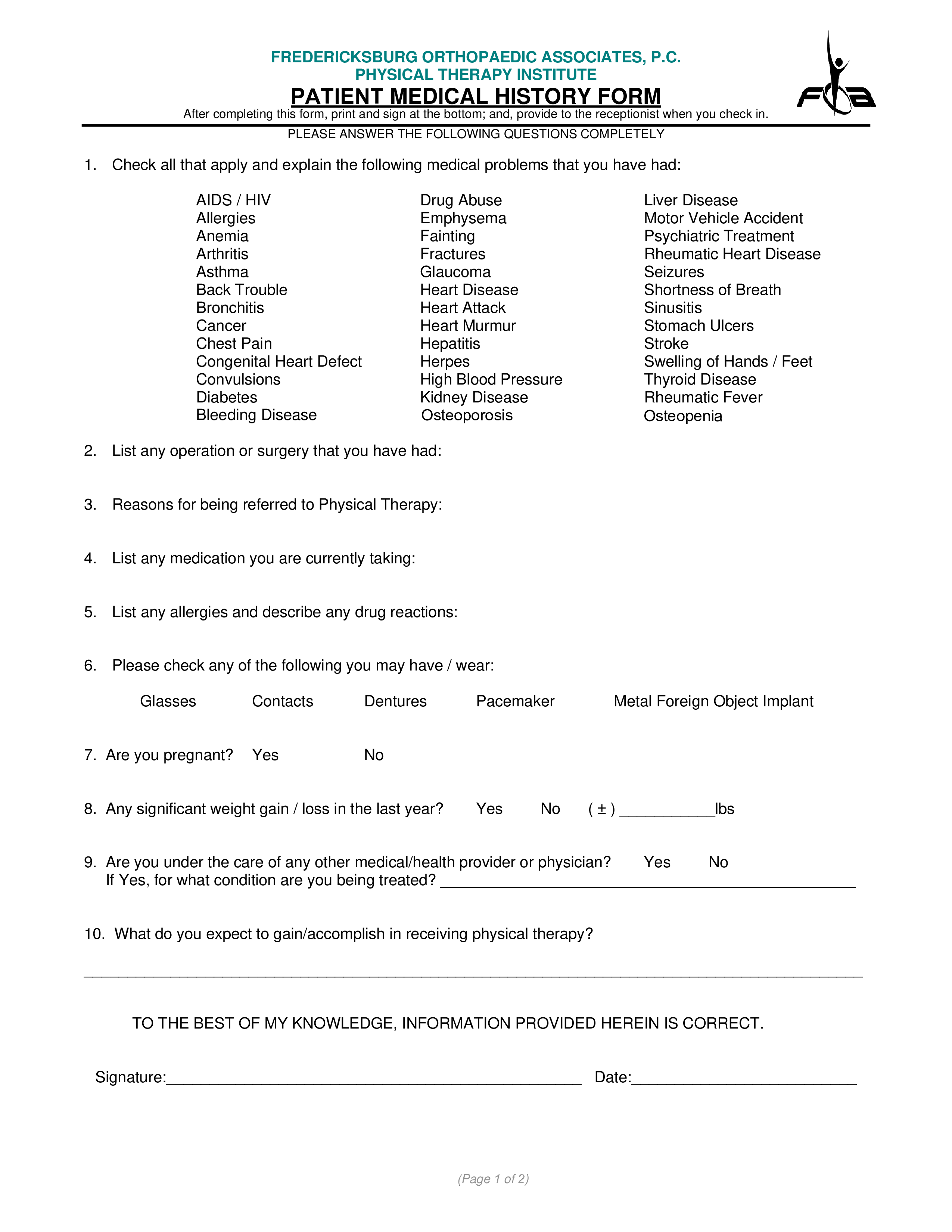
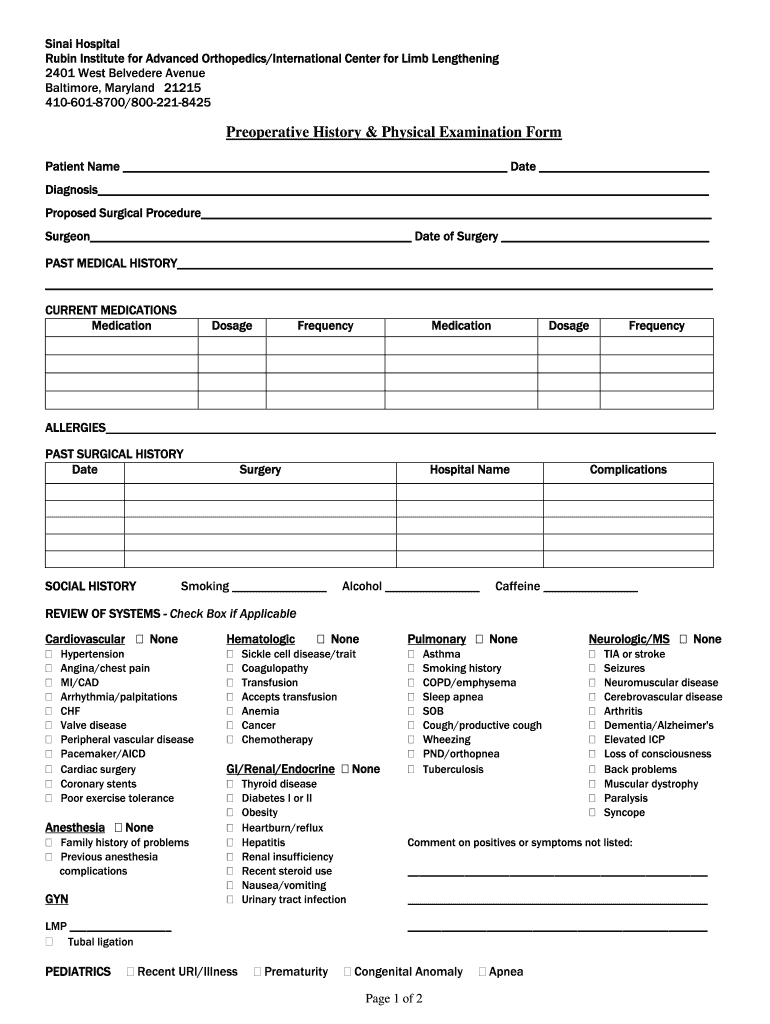
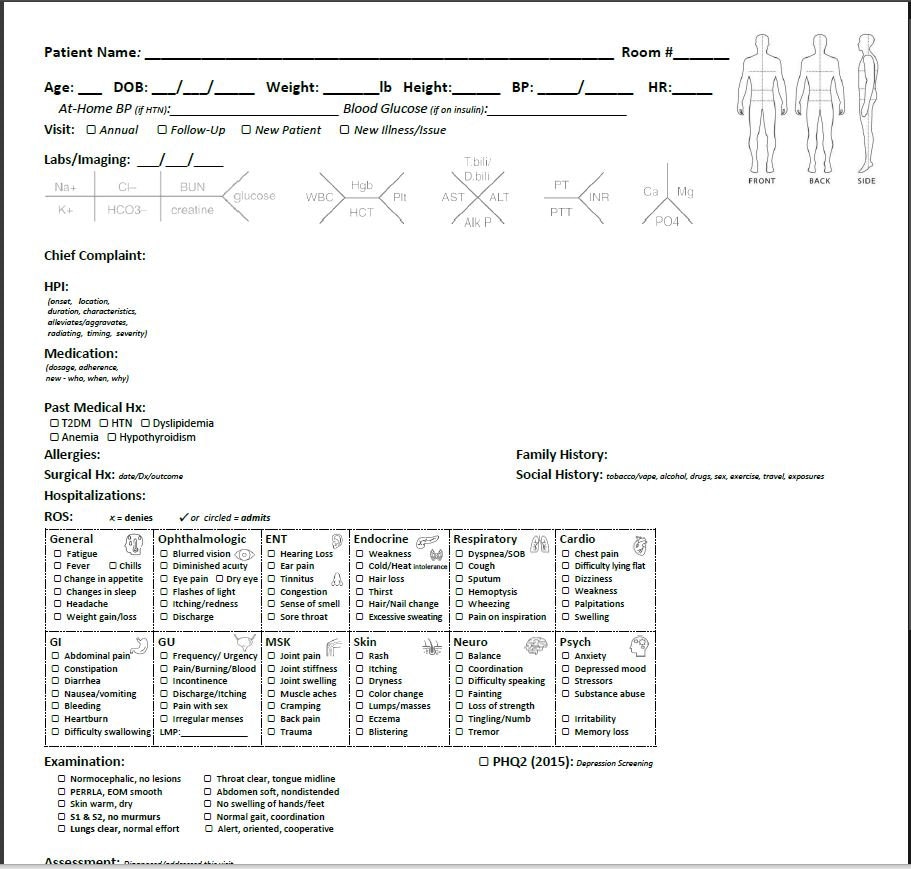
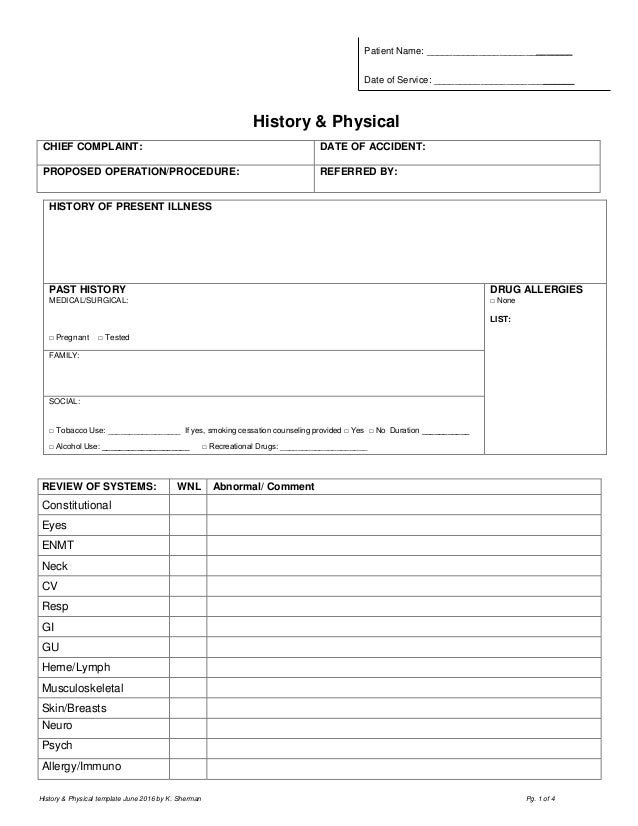
History And Physical Template - Web as a tool to teach this critical aspect of medicine, students are required to complete and submit to the clerkship office six detailed history and physical examinations. The students have granted permission to have these h&ps posted on the website as examples. The form covers the patient’s personal medical history, such as diagnoses, medication, allergies, past diseases, therapies, clinical research, and that of their family. “i got lightheadedness and felt too weak to walk” source and setting: Further diagnostic investigations—imaging, blood tests, pulmonary function studies, and even parts of the physical examination—depend on the history. History & physical short form / procedure. It outlines a plan for addressing the issues which prompted the hospitalization. This is the first admission for this 56 year old woman, who states she was in her usual state of good health until one week prior to admission. She was first admitted to cpmc in 1995 when she presented with a complaint of intermittent midsternal chest pain. History and physical is the most formal and complete assessment of the patient and the problem. Ucla form #201539 rev (10/14) page 1 of 1. It is an important reference document that provides concise information about a patient's history and exam findings at the time of admission. Further diagnostic investigations—imaging, blood tests, pulmonary function studies, and even parts of the physical examination—depend on the history. Your ability to gather a sensitive and nuanced history and to perform a thorough and accurate examination deepens your relationships with patients, focuses Skin bruising, discoloration, pruritus, birthmarks, moles, ulcers, decubiti, changes in the hair or nails, sun exposure and protection. Web comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: The history was obtained from both the patient’s mother and grandmother, who are both considered to be reliable historians. The form covers the patient’s personal medical history, such as diagnoses, medication, allergies, past diseases, therapies, clinical research, and that of their family. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Web a history and physical form is a foundational document healthcare professionals use to gather comprehensive information about a patient's medical history and current health status through a physical examination. Web history of present illness. Web this document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs, and physical examination findings. It is an important reference document that provides concise information about a patient's history and exam findings at the time of admission. U or iu, trailing zeros (1.0) or leading zeros (.1), ms or mso4, mgso4, da or dop, db, or dob, qd or qod, snp. Prescribed drugs and other medications; Outline an organized approach to the patient’s problem that reflects a review of the pertinent literature. Ucla form #201539 rev (10/14) page 1 of 1. This is the first admission for this 56 year old woman, who states she was in her usual state of good health until one week prior to admission. Web sample pediatric history and physical exam. Web it is the responsibility of the organized medical staff to determine the minimum required content of medical history and physical (h & p) examinations (see ms.03.01.01 ep 6). Your ability to gather a sensitive and nuanced history and to perform a thorough and accurate examination deepens your relationships with patients, focuses (please check all conditions that you have or have had) none. Prescribed drugs and other medications; Web sample pediatric history and physical exam. Web it is the responsibility of the organized medical staff to determine the minimum. Outline an organized approach to the patient’s problem that reflects a review of the pertinent literature. Web this document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs, and physical examination findings. (please check all conditions that you have or have had) none. Web a. The history was obtained from both the patient’s mother and grandmother, who are both considered to be reliable historians. Outline an organized approach to the patient’s problem that reflects a review of the pertinent literature. The documentation template includes the following sections: History and physical is the most formal and complete assessment of the patient and the problem. The form. Web in a focused history and physical, this exhaustive list needn’t be included. Outline an organized approach to the patient’s problem that reflects a review of the pertinent literature. Chief complaint, history of present illness, review of systems, sexual. It is an important reference document that provides concise information about a patient's history and exam findings at the time of. It is an important reference document that provides concise information about a patient's history and exam findings at the time of admission. This is the first admission for this 56 year old woman, who states she was in her usual state of good health until one week prior to admission. Web a history and physical form is a foundational document. It is an important reference document that provides concise information about a patient's history and exam findings at the time of admission. Web it is the responsibility of the organized medical staff to determine the minimum required content of medical history and physical (h & p) examinations (see ms.03.01.01 ep 6). Web history and physical examination (h&p) examples. Outline an. Web the written history and physical (h&p) serves several purposes: H&p is shorthand for the formal document that physicians produce through the interview with the patient, the physical exam, and the summary of the testing either obtained or pending. Skin bruising, discoloration, pruritus, birthmarks, moles, ulcers, decubiti, changes in the hair or nails, sun exposure and protection. The form covers. The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Outline an organized approach to the patient’s problem that reflects a review of the pertinent literature. “i got lightheadedness and felt too weak to walk” source and setting: Web specific details from the history raise the probability of different diagnoses and direct further tests. History & physical short form / procedure. Date and time of h&p: Enter fin (not mrn) state your name, patient name, patient mrn and fin, admitting attending, date of service date: Web accurately and completely write up a patient history and physical. Skin bruising, discoloration, pruritus, birthmarks, moles, ulcers, decubiti, changes in the hair or nails, sun exposure and protection. Enter fin (not mrn) state your name, patient name, patient mrn and fin, admitting attending, date of service date: Your ability to gather a sensitive and nuanced history and to perform a thorough and accurate examination deepens your relationships with patients, focuses Web in a focused history and physical, this exhaustive list needn’t be included. Web history & physical short. Further diagnostic investigations—imaging, blood tests, pulmonary function studies, and even parts of the physical examination—depend on the history. Web as a tool to teach this critical aspect of medicine, students are required to complete and submit to the clerkship office six detailed history and physical examinations. (please check all conditions that you have or have had) none. Web transcribed medical transcription history and physical work type sample reports for reference by medical transcriptionists and allied health professionals. Your ability to gather a sensitive and nuanced history and to perform a thorough and accurate examination deepens your relationships with patients, focuses History & physical short form / procedure. Web this study gathers validity evidence of an expanded history and physical examination (h&p 360) to address chronic diseases through incorporation of biopsychosocial elements that are lacking in traditional h&p assessments via a multisite randomized controlled trial among medical students. “i got lightheadedness and felt too weak to walk” source and setting: The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Web specific details from the history raise the probability of different diagnoses and direct further tests in a productive manner. Web history of present illness. Web a general medical history form is a document used to record a patient’s medical history at the time of or after consultation and/or examination with a medical practitioner. It is an important reference document that provides concise information about a patient's history and exam findings at the time of admission. Outline an organized approach to the patient’s problem that reflects a review of the pertinent literature. Web history & physical short form / procedure. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy.Printable History And Physical Form Template Printable Templates
History And Physical Template Word
History And Physical Template Word
Printable Medical History And Physical Form
History And Physical Form Template Pdf Template vrogue.co
History And Physical Template
History And Physical Template
History & Physical Exam Template Printable and Editable Versions Etsy
Printable History And Physical Form Template Printable Templates
History And Physical Template Word
Web Comprehensive Adult History And Physical (Sample Summative H&P By M2 Student) Chief Complaint:
Web This Document Contains A Patient Intake Form Collecting Demographic Information, Chief Complaint, History Of Present Illness, Review Of Systems, Past Medical History, Social History, Vital Signs, And Physical Examination Findings.
Skin Bruising, Discoloration, Pruritus, Birthmarks, Moles, Ulcers, Decubiti, Changes In The Hair Or Nails, Sun Exposure And Protection.
The Form Covers The Patient’s Personal Medical History, Such As Diagnoses, Medication, Allergies, Past Diseases, Therapies, Clinical Research, And That Of Their Family.
Related Post: