Mental Health Soap Note Template
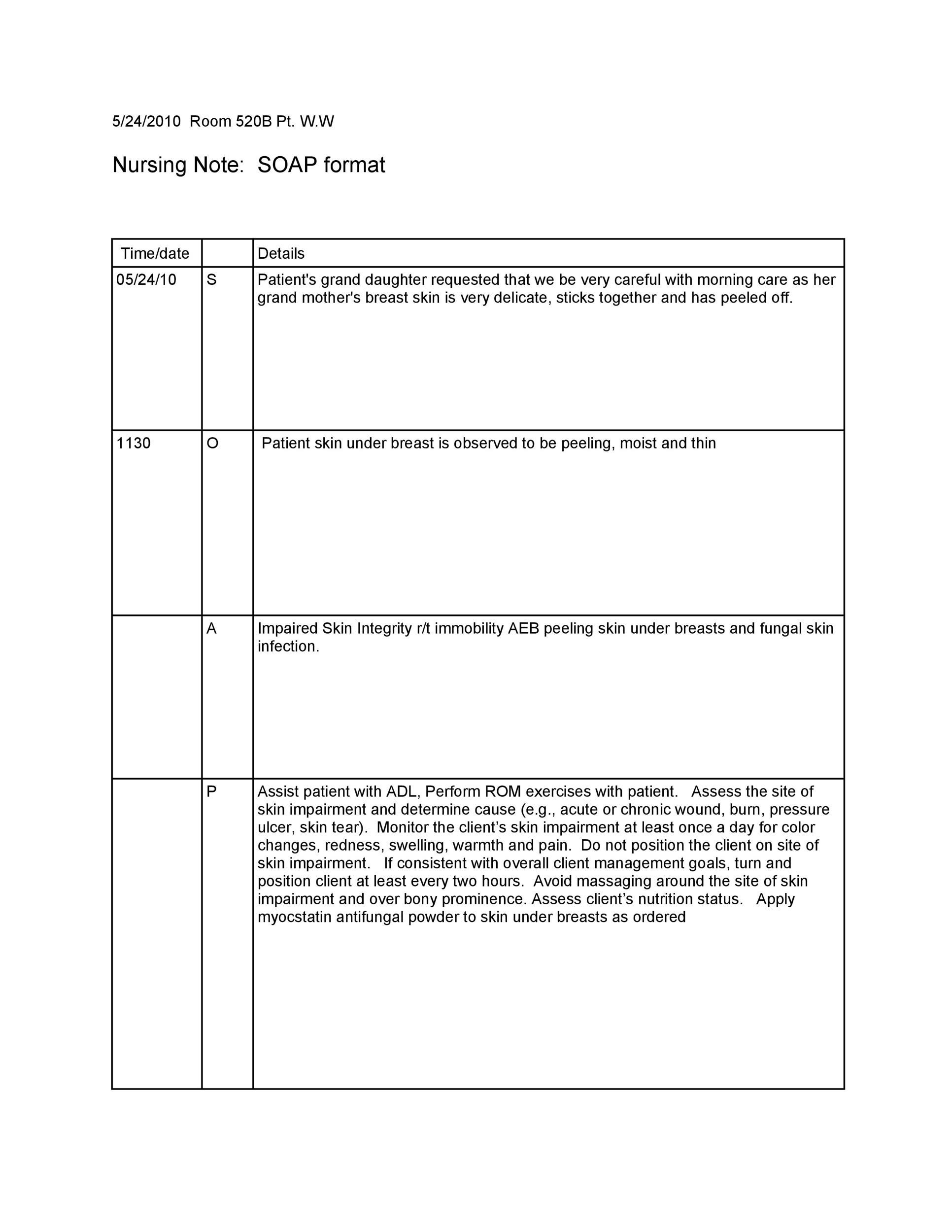
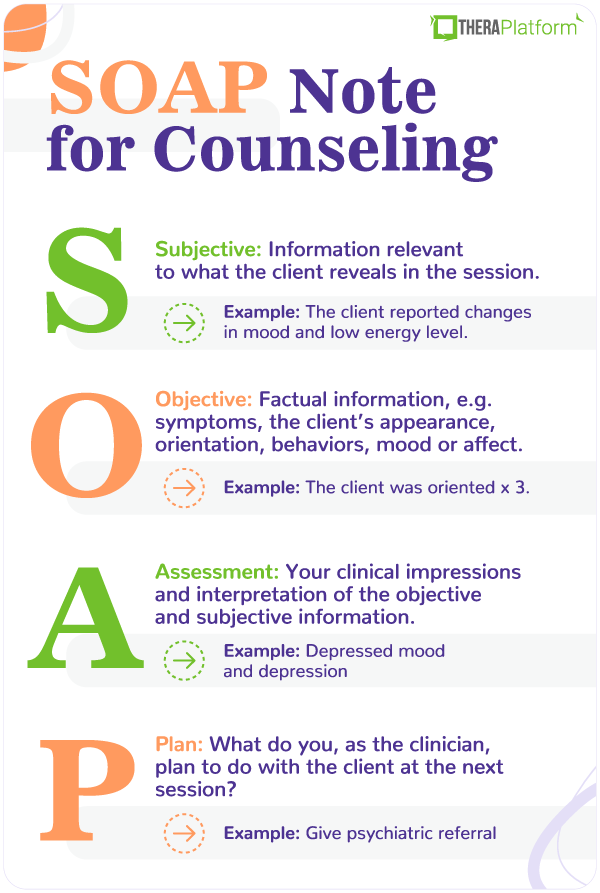
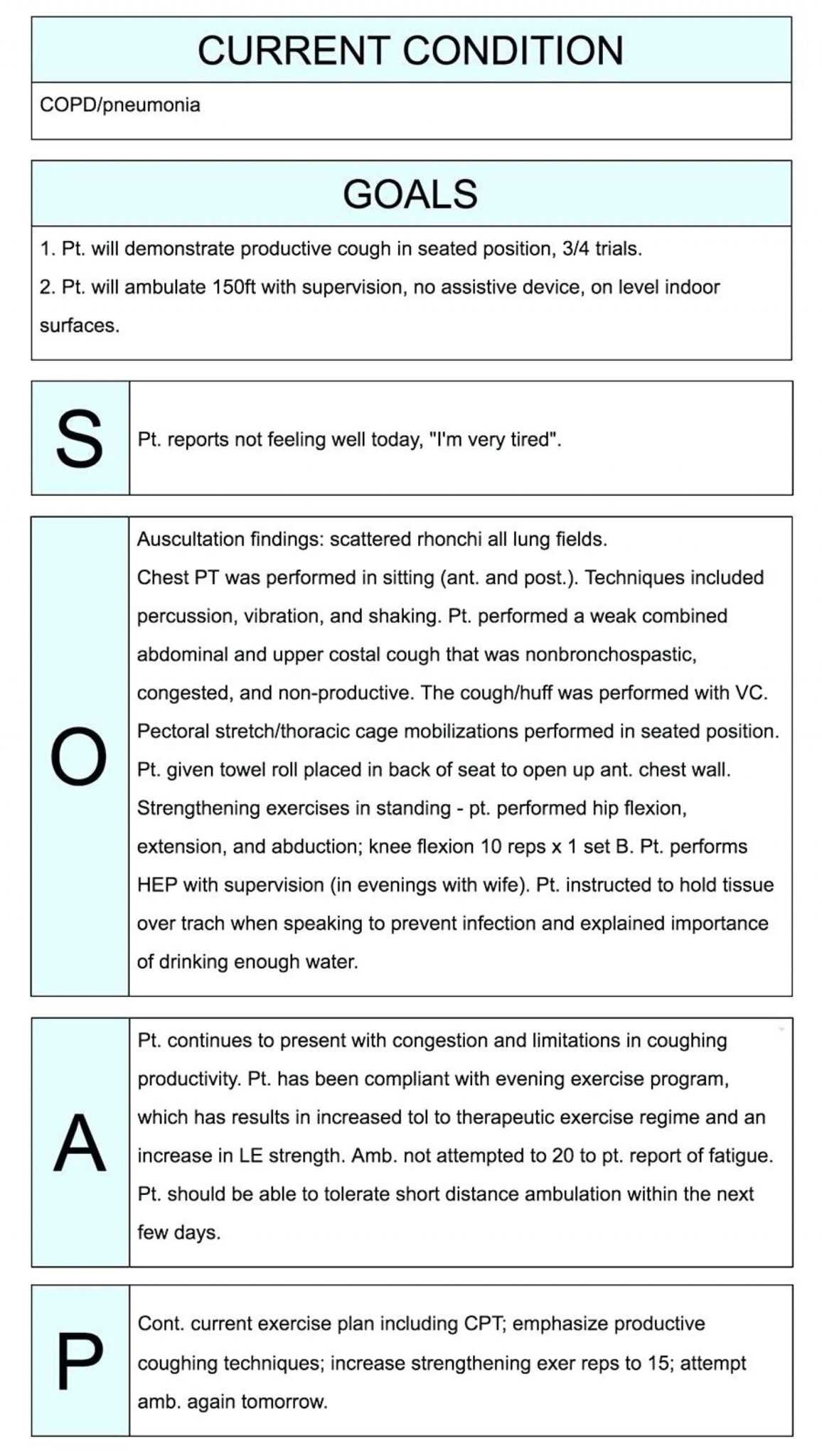
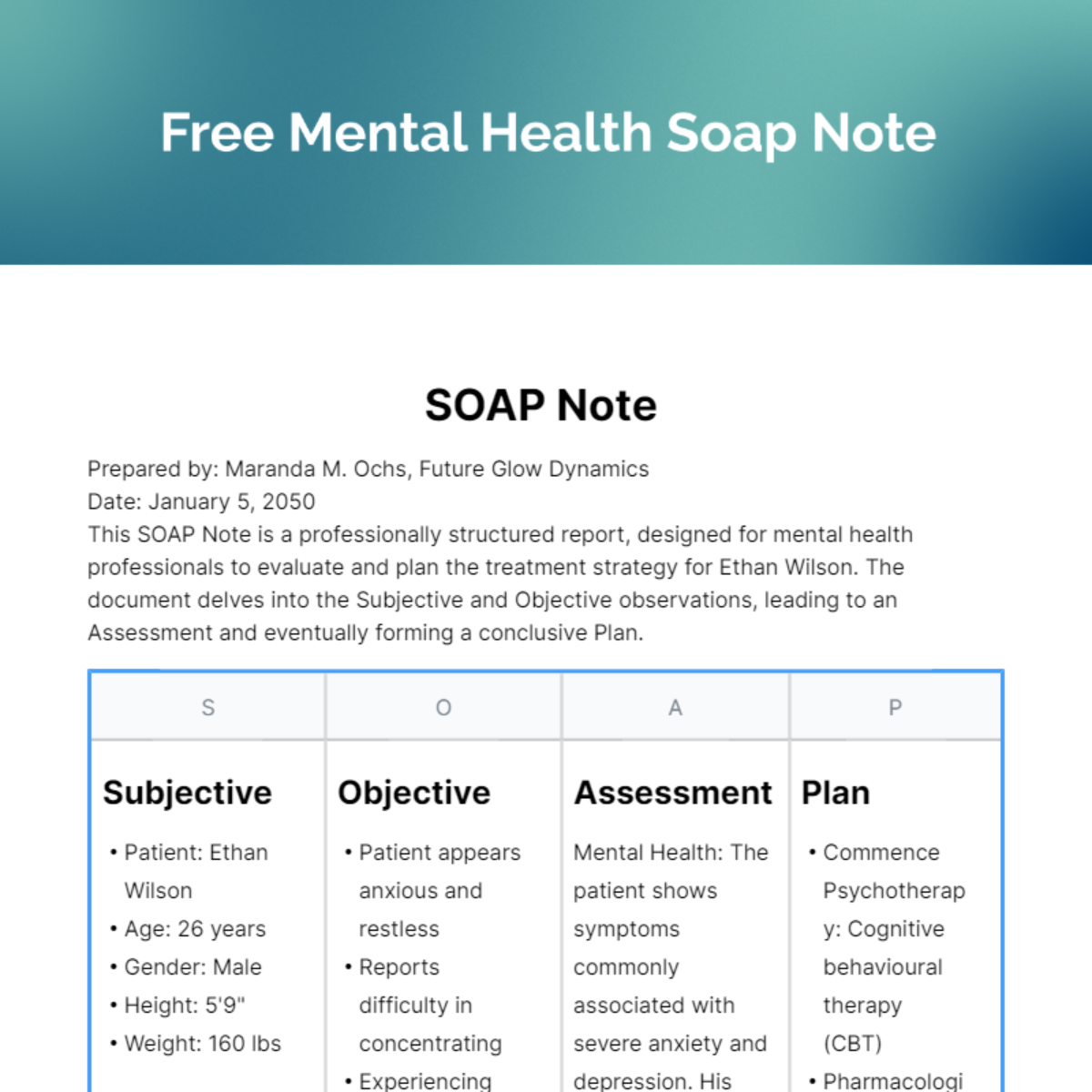
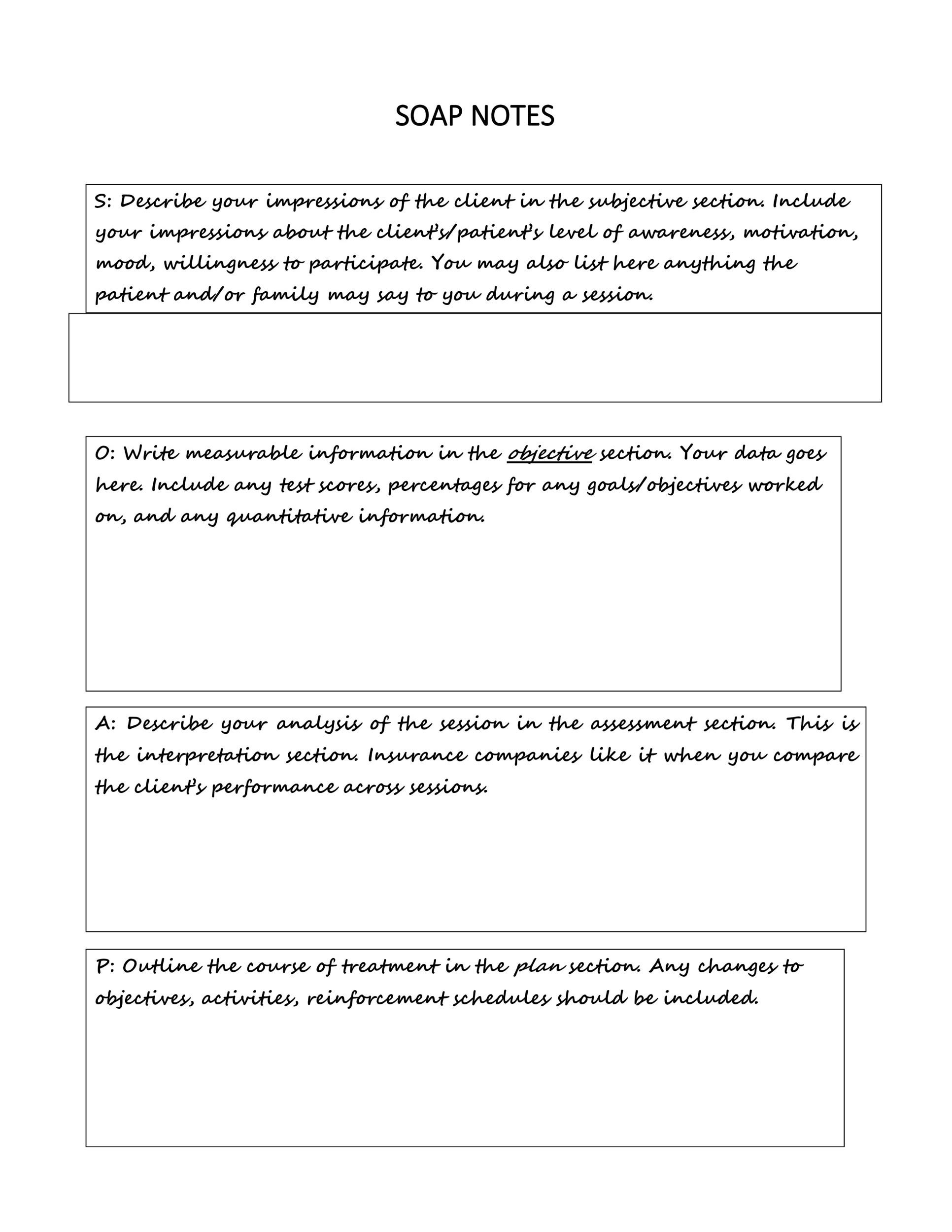
Mental Health Soap Note Template - This guide provides a thorough overview of soap notes, their purpose, and essential elements tailored for pmhnps. See examples of soap note templates and tips for effective documentation. Web learn what soap notes are, why they are important, and how to write them for mental health professionals. Web learn how to use the soap note format to document your behavioral health sessions effectively. Web download a free pdf template for soap notes, a common clinical documentation format for mental health professionals. Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. See examples of subjective, objective, assessment, and plan sections for a client with depression. See examples of soap notes for different client scenarios and contexts. Find examples of clinical, soap, and dap notes for different specialties and modalities. Web learn how to write effective soap notes for mental health sessions with this guide. Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. Download a free soap note template and see a sample note based on a therapy scenario. Web learn how to write effective soap notes for mental health counselling using a systematic approach and a free pdf template. They include subjective, objective, assessment, and plan components. See examples of subjective, objective, assessment, and plan sections for a client with depression. The client presents for therapy, wanting to work on symptoms associated with their borderline personality disorder diagnosis. In the realm of therapy, documentation like soap notes isn’t just a formality—it’s a critical component of effective client care. See examples of soap note templates and tips for effective documentation. See examples of soap notes for different client scenarios and contexts. Download a free editable pdf template to organize your client sessions and progress. Soap notes help you organize, analyze, plan, and document your client's treatment progress. Web learn how to use soap notes, a framework to organise treatment information of a client in a highly structured format. Web learn how to write soap notes for mental health, a standardized documentation format for therapists and healthcare providers. Web learn what soap notes are and how to write them for mental health patients. Web looking for therapy soap note examples? Web learn how to write soap notes for mental health patients with this guide. Web learn what soap notes are and how to write them for anxiety and depression. Download a free soap note template and see a sample note based on a therapy scenario. It provides context for the assessment and plan sections. Web soap notes are a structured way of documenting client information and progress in counseling sessions. Here are 3 free, downloadable soap note examples with templates to help write effective soap notes. They include subjective, objective, assessment, and plan components. See examples of soap note templates and tips for effective documentation. Web learn how to use progress note templates to document client progress in mental health, therapy, and counseling settings. Web learn how to use the. Web learn what soap notes are, how to write them, and when to use them for mental health documentation. Find examples of clinical, soap, and dap notes for different specialties and modalities. Determine the chief complaint (cc) or presenting problem. Web learn how to use the soap note format to document your behavioral health sessions effectively. Learn what soap stands. Web learn what soap notes are, why they are important, and how to write them for mental health professionals. Web soap notes are a structured way of documenting client information and progress in counseling sessions. Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health. See examples, best practices, and tips for each section of soap notes: Web learn how to write soap notes for mental health, a standardized documentation format for therapists and healthcare providers. Download a free pdf template or use a digital tool to access, share, and report your notes anytime and anywhere. Web download a free soap notes template pdf file. Web learn how to use a soap note template to document and improve mental health care. Web learn how to use soap notes, a framework to organise treatment information of a client in a highly structured format. They include subjective, objective, assessment, and plan components. Learn how to write soap notes and see examples and templates. Web learn how to. See examples, best practices, and tips for each section of soap notes: Download a free editable pdf template to organize your client sessions and progress. Web learn what soap notes are, how to write them, and when to use them for mental health documentation. Web learn how to write effective soap notes for mental health sessions with this guide. To. Web learn what soap notes are and how to write them for anxiety and depression. Web learn how to write soap notes for mental health patients with this guide. See examples of subjective, objective, assessment, and plan sections for a client with depression. Here are 3 free, downloadable soap note examples with templates to help write effective soap notes. Find. See examples, compare with dap and birp notes, and find out how to automate progress notes with ai. Web learn what soap notes are, how to write them, and when to use them for mental health documentation. The client presents for therapy, wanting to work on symptoms associated with their borderline personality disorder diagnosis. Download a free pdf template or. Web learn what soap notes are and how to write them for behavioral health care professionals. Download a free editable pdf template to organize your client sessions and progress. Subjective, objective, assessment, and planning. Subjective, objective, assessment, and plan. See examples of subjective, objective, assessment, and plan sections for a client with depression. This guide provides a thorough overview of soap notes, their purpose, and essential elements tailored for pmhnps. Web learn how to use soap notes, a framework to organise treatment information of a client in a highly structured format. Find examples of clinical, soap, and dap notes for different specialties and modalities. Learn how to write soap notes and see examples. Web streamline your soap note documentation with our cheat sheet tailored for therapists. Web soap (subjective, objective, assessment, and plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. Learn how to use the template, who can benefit from it, and what are the benefits of soap notes. Subjective, objective, assessment, and planning. Subjective, objective, assessment, and plan. Web soap notes are a structured way of documenting client information and progress in counseling sessions. Web learn how to write soap notes for mental health, a standardized documentation format for therapists and healthcare providers. See examples and templates for each section of soap notes: Web soap note template and example. A soap note has four sections and an example is provided below. Web learn how to use a soap note template to document and improve mental health care. To gather relevant information, healthcare providers should: Determine the chief complaint (cc) or presenting problem. Web learn what soap notes are and how to write them for mental health patients. See examples of soap notes for different client scenarios and contexts. Find examples and templates for different therapeutic sectors, and how to use.Soap Notes Template Counseling
023 Soap Note Example Mental Health Ems Format Template inside Soap
Sample Mental Health Assessment Report Mental health assessment, Soap
FREE SOAP Note Templates Templates & Examples Edit Online & Download
Soap Note Template Social Work
Free Mental Health SOAP Note Template PDF SafetyCulture
Soap Note Template Mental Health Pdf
Mental Health Soap Note Template
Psychotherapy Soap Note Template
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
Web Looking For Therapy Soap Note Examples?
They Include Subjective, Objective, Assessment, And Plan Components.
The Subjective Section Of The Soap Note Captures The Patient's Subjective Experiences, Personal Views, And Feelings.
Find Out What Each Letter Stands For, Why Soap Notes Are Important, And See Examples Of Basic Templates.
Related Post:




.png)