Psychiatric History Template
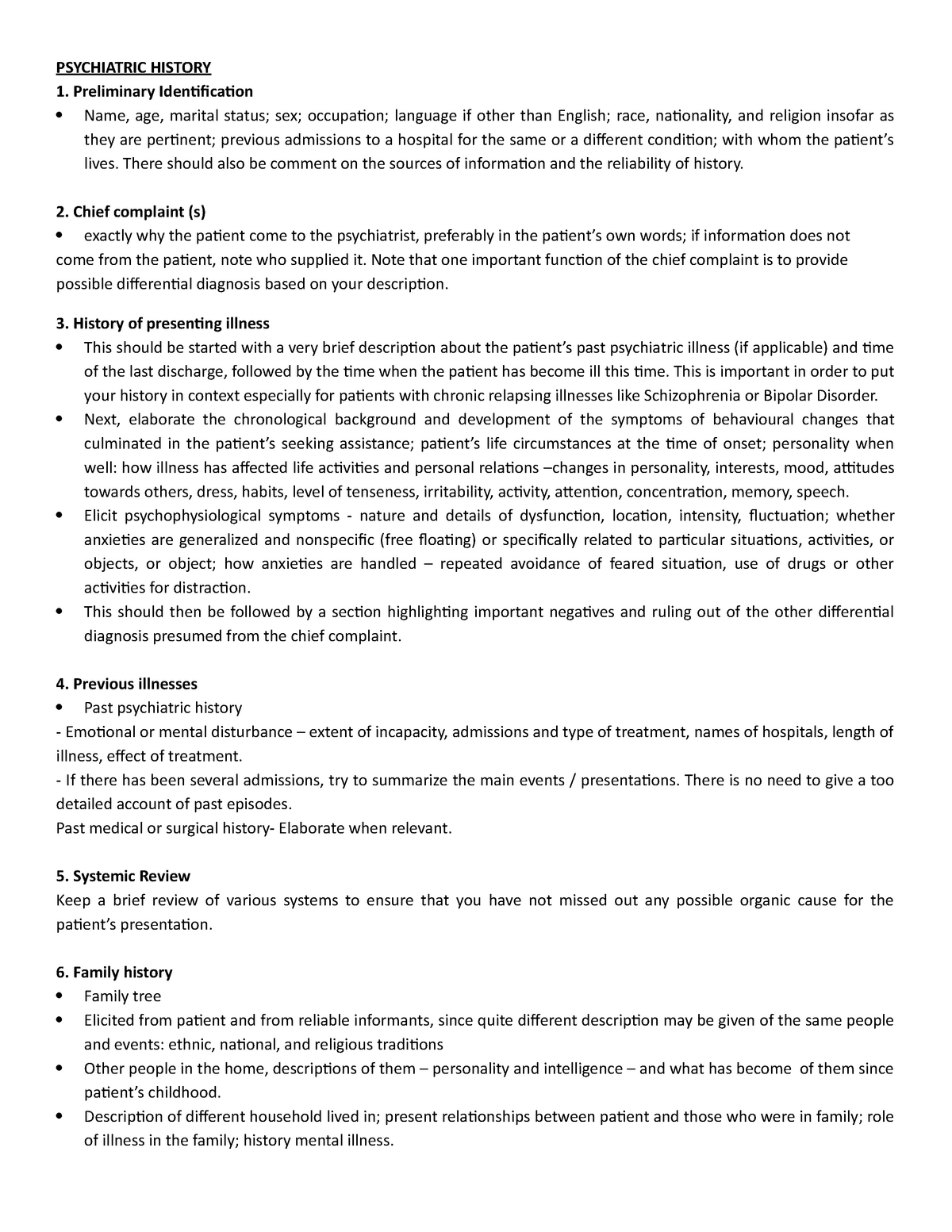
Psychiatric History Template - In addition, general principles to guide the conduct of evaluations Web what should you include in your initial psychiatric evaluation? Web for each domain—appearance, speech, mood, affect, thought, perception, intelligence, cognition, rapport, and insight—a chapter is devoted to description of the many more common as well as less common signs and symptoms that are germane to psychiatric assessment. • a logical roadmap starting with the presenting complaint, through previous history, personal history, and up to the current situation. It should include information about the patient's history, symptoms, any relevant physical or psychological examination findings, any data from rating scales or laboratory studies, and a thorough. Web this document outlines a psychiatric history taking format that includes: 1) general psychiatric evaluation, 2) emergency evaluation, and 3) clinical consultation. This involves summarising the key features of the history, mse and risk assessment, as well as (differential) diagnosis and management plan. Download the depression history taking pdf osce checklist, or use our interactive osce checklist. Click on the links to be taken to the online resource. The history taking and risk assessment video and the mental state examination video feature extracts from patient interviews (conducted by dr jan melichar), divided into sections to illustrate various stages of the interview. The details of referral several years ago is part of the person’s past psychiatric. Web this guide will provide a structured approach for taking a generic psychiatric history, which can then be adapted based on the individual presentation. The key is to start with their current well being not when they were referred several years ago. Each template can be customized to fit individual needs, and new ones are continuously added to the library. Web assessment of psychiatric symptoms and psychiatric treatment history is by definition a core activity of an initial psychiatric evaluation. Web this guide provides examples of questions that may be useful in exploring first rank symptoms when taking a psychiatric history. Web osmind simplifies the process of writing psychiatry progress notes with over 60 templates tailored to for mental health clinicians. Identifying information about the patient and details of their chief complaint and history of present illness. Web after completing your psychiatric assessment it is time to formulate the case. Web a thorough phipps history allows a deep understanding of a patient’s life and facilitates a detailed formulation using the perspectives of psychiatry approach. Consider taking a collateral history. chief complaint (this can be in the patient’s own words or a brief description of why they are coming in for an evaluation). Explore the patient's ideas, concerns and expectations. This involves summarising the key features of the history, mse and risk assessment, as well as (differential) diagnosis and management plan. Web psychiatric evaluations are discussed: Excess concern with appearance or certain part of body avoidance behavior. Web the patient’s psychiatric treatment history: If not, information is sought from family, caregivers, or other collateral sources (eg, police). Web what should you include in your initial psychiatric evaluation? Collateral information regarding all past psychiatric history is. The details of referral several years ago is part of the person’s past psychiatric. Guide to psychiatric history taking by the university of. Web this guide provides examples of questions that may be useful in exploring first rank symptoms when taking a psychiatric history. This page is devoted to online resources around. you’ll want to have a template that includes the following sections: Web a common problem that medical students experience is how to write up the history of presenting complaint in the person seen in a community mental health setting. Web this guide provides examples of questions that may be useful in exploring first rank symptoms when taking a psychiatric. Each template can be customized to fit individual needs, and new ones are continuously added to the library. Web an initial psychiatric evaluation note with all components of the initial evaluation including history of present illness, past medical history, social history, mental status examination, diagnostic impressions, and treatment plan. Explore the patient's ideas, concerns and expectations. 1) general psychiatric evaluation,. The physician must determine whether the patient can provide a history, ie, whether the patient readily and coherently responds to initial questions. Web assessment of psychiatric symptoms and psychiatric treatment history is by definition a core activity of an initial psychiatric evaluation. You may also be interested in our mental state examination (mse) or exploring first rank symptoms guides. Some. Download the depression history taking pdf osce checklist, or use our interactive osce checklist. • a logical roadmap starting with the presenting complaint, through previous history, personal history, and up to the current situation. Web this guide provides a structured approach to taking a depression history in an osce setting. chief complaint (this can be in the patient’s own. It should include information about the patient's history, symptoms, any relevant physical or psychological examination findings, any data from rating scales or laboratory studies, and a thorough. Explore the patient's ideas, concerns and expectations. Web history taking and clinical skills in psychiatry. The history taking and risk assessment video and the mental state examination video feature extracts from patient interviews. This template is used for conducting an initial evaluation of a patient's mental health condition. Web the patient’s psychiatric treatment history: This involves summarising the key features of the history, mse and risk assessment, as well as (differential) diagnosis and management plan. It should include information about the patient's history, symptoms, any relevant physical or psychological examination findings, any data. Web this guide provides a structured approach to taking a depression history in an osce setting. Excess concern with appearance or certain part of body avoidance behavior. The details of referral several years ago is part of the person’s past psychiatric. Identifying information about the patient and details of their chief complaint and history of present illness. This page is. Web this guide will provide a structured approach for taking a generic psychiatric history, which can then be adapted based on the individual presentation. Web this guide provides examples of questions that may be useful in exploring first rank symptoms when taking a psychiatric history. Some areas covered in a general psychiatric history will also form part of. Medical and. Click on the links to be taken to the online resource. Consider taking a collateral history. Some areas covered in a general psychiatric history will also form part of. Web give you a starting point to work from as you learn to take a psychiatric history and do a mental state examination. Web evaluate how severe the patient’s illness was,. Consider taking a collateral history. • a logical roadmap starting with the presenting complaint, through previous history, personal history, and up to the current situation. In addition, general principles to guide the conduct of evaluations Click on the links to be taken to the online resource. Download the depression history taking pdf osce checklist, or use our interactive osce checklist. Web for each domain—appearance, speech, mood, affect, thought, perception, intelligence, cognition, rapport, and insight—a chapter is devoted to description of the many more common as well as less common signs and symptoms that are germane to psychiatric assessment. Exploring the patient's past psychiatric, medical, family, personal, and substance use histories to understand any relevant context. Collateral information regarding all past psychiatric history is. you’ll want to have a template that includes the following sections: Web updated 2024 with viva questions & psychiatric history osce stations. Other core activities include identifying the reason that the patient is presenting for evaluation and understanding the patient’s background, relationships, life circumstances, and strengths and. Excess concern with appearance or certain part of body avoidance behavior. Web a thorough phipps history allows a deep understanding of a patient’s life and facilitates a detailed formulation using the perspectives of psychiatry approach. Web psychiatric evaluations are discussed: Identifying information about the patient and details of their chief complaint and history of present illness. The key is to start with their current well being not when they were referred several years ago.Sample Demographics and Psychiatric/Health History (in Percentages
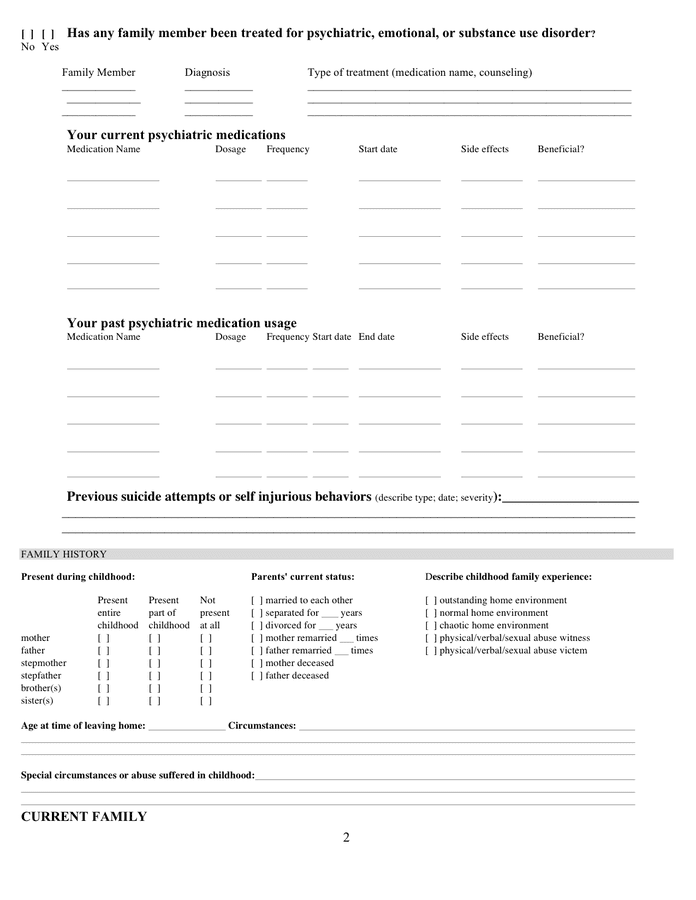
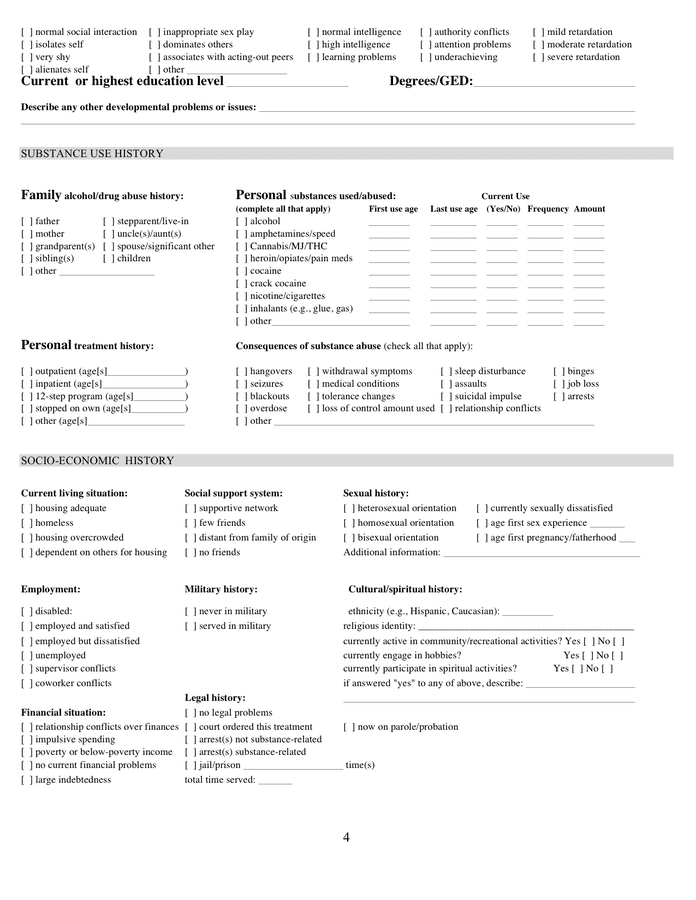
Medical psychiatric history form in Word and Pdf formats page 2 of 4
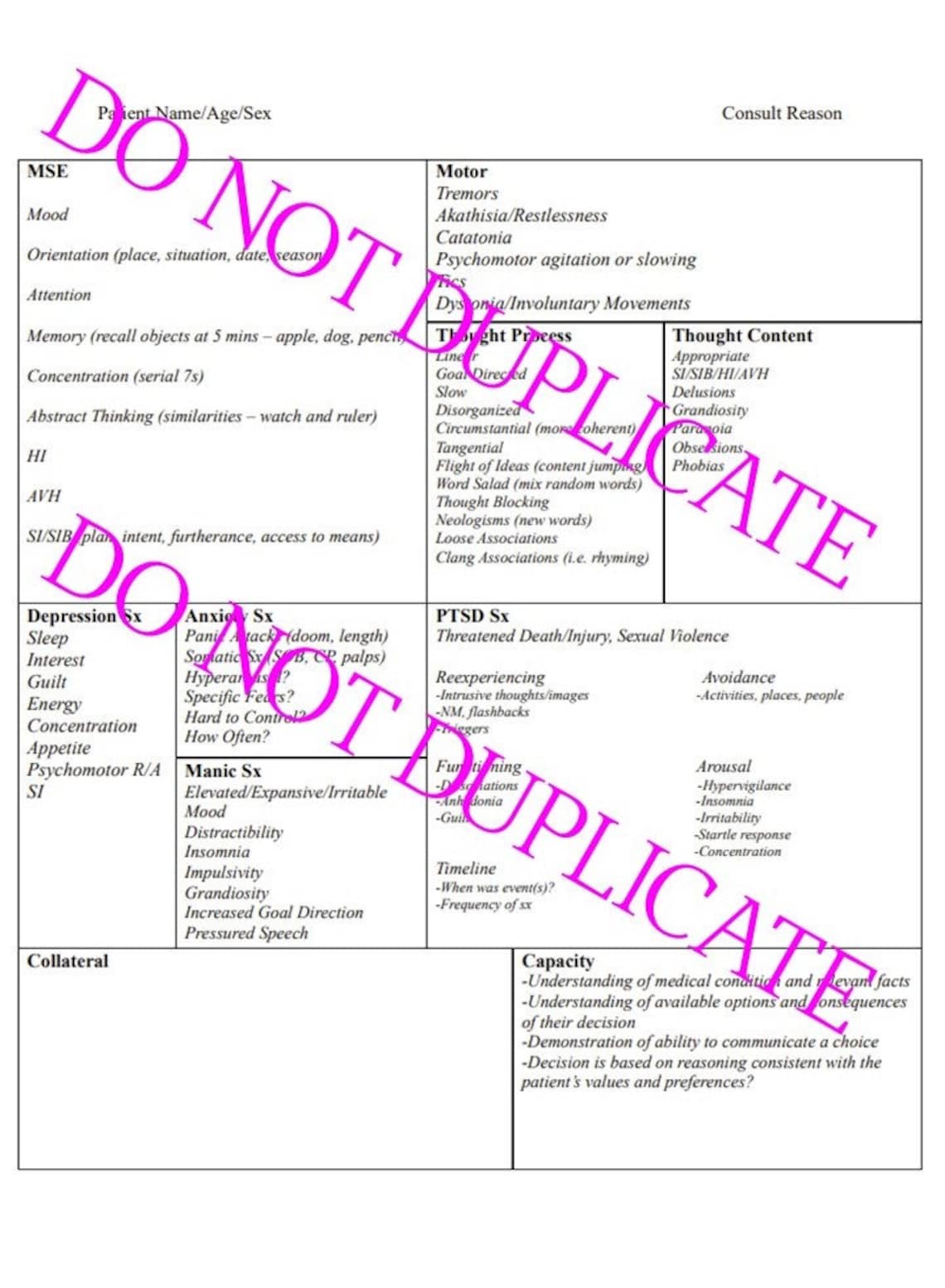
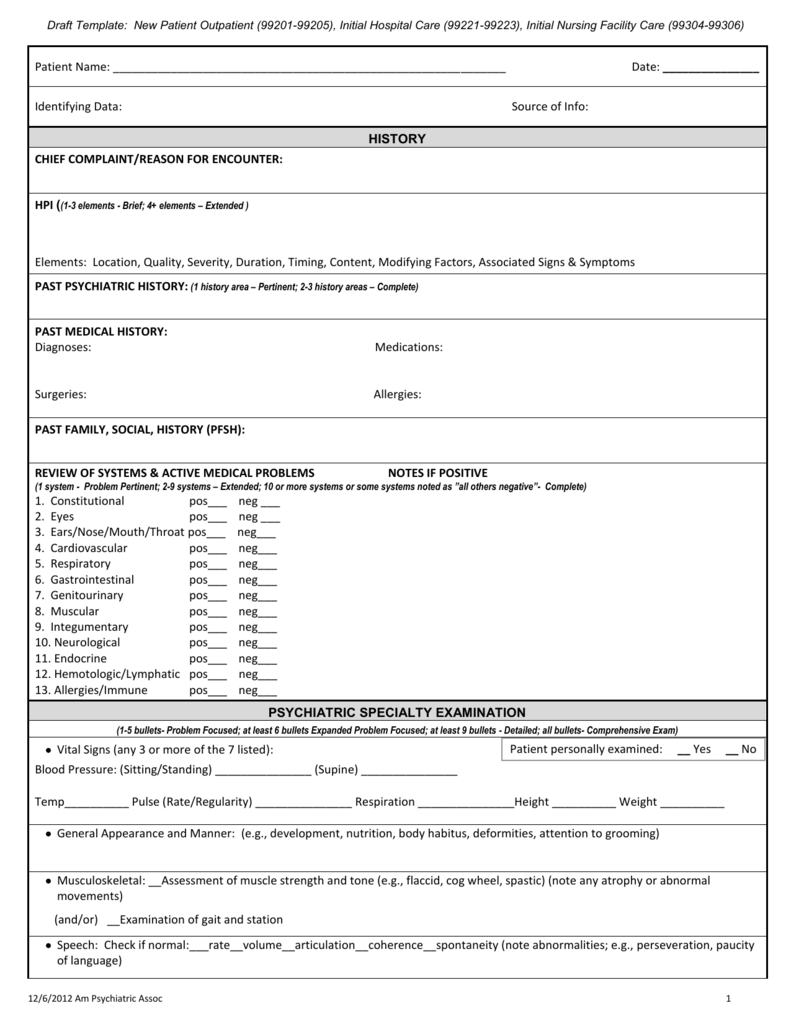
Psychiatry HPI Template Psych History Psychiatric H&P Assessment
Medical psychiatric history form in Word and Pdf formats page 3 of 4
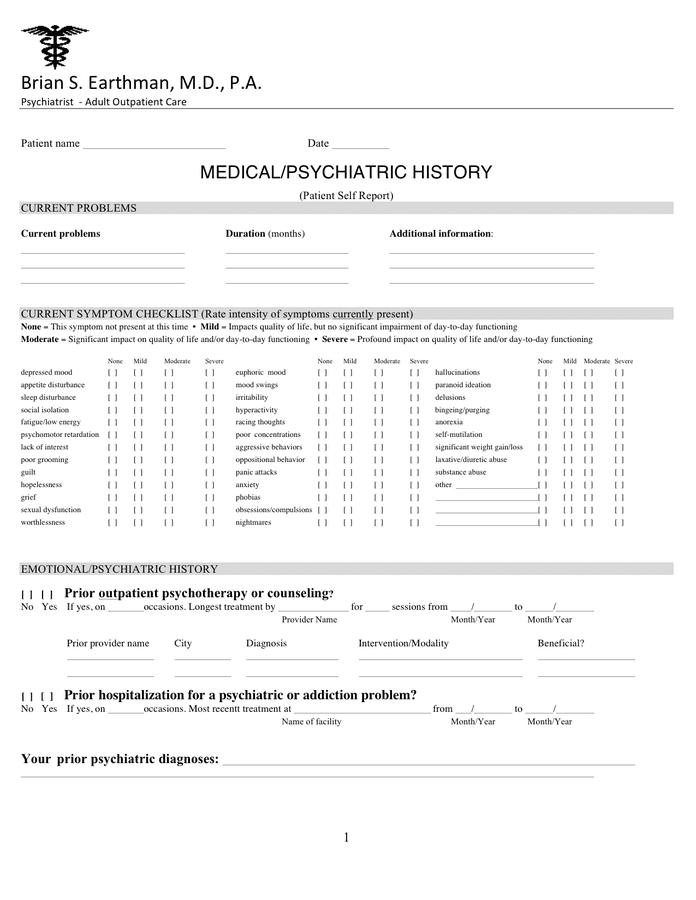
Medical psychiatric history form in Word and Pdf formats
3. Psychiatric History Doc Template pdfFiller
Psychiatric History Template
Medical psychiatric history form in Word and Pdf formats page 4 of 4
Printable Psychiatric History Taking Template Templat vrogue.co
Psychiatric History And Physical Template Flyer Template
Web What Should You Include In Your Initial Psychiatric Evaluation?
Web This Guide Provides Examples Of Questions That May Be Useful In Exploring First Rank Symptoms When Taking A Psychiatric History.
The History Taking And Risk Assessment Video And The Mental State Examination Video Feature Extracts From Patient Interviews (Conducted By Dr Jan Melichar), Divided Into Sections To Illustrate Various Stages Of The Interview.
Some Areas Covered In A General Psychiatric History Will Also Form Part Of.
Related Post: